Is Gluten Really the #1 Food Enemy? Yes, No . . . Maybe
On my podcast, The Smartest Doctor in the Room, I had an in-depth conversation with Dr. Peter Green an expert on gluten-related disorders.
What you will hear may surprise you: not everyone has to avoid foods containing gluten.
What to Avoid if You are Sensitive to Gluten
However, if you are sensitive to gluten these are the foods you need to avoid:
- wheat
- barley
- rye
Just be aware it’s not just bread that contains these grains – you also have to watch out for cakes, cookies, pasta, soy sauce, and even beer!
Do You Have a Wheat Allergy?
Unlikely. Wheat allergy is actually very rare.
Over the years, I have had many patients request a wheat allergy test, almost all of which came out negative. In fact, I have only seen one case in my 25 years of practice. The actual statistics show only 3% in children and 0.3% in adults.
The one patient I saw, which I mention on the podcast, was actually a baker’s daughter. She not only worked in the bakery growing up, but the family lives above the bakery. She was inhaling wheat flour her whole life. Then one day she ate a slice of pizza and started wheezing and couldn’t have any food with wheat again! I felt bad for her because she said: “I’m Italian, I can’t be allergic to pasta!”
Celiac Disease – The More Common Culprit
However, because the Celiac disease is now known to be more common than once thought, I have started checking blood tests for gluten-sensitivity. I have found many patients who would be better off gluten, which includes wheat, barley, rye and many types of oats.
Celiac disease can be a much more subtle cause of illness and in the past was frequently overlooked.
When I was in medical school we were basically taught that Celiac disease is a pediatric disease. The young children would have big bellies but appear malnourished from constant diarrhea. Their intestines are damaged by gluten and cause dramatic sickness.
I used to think that the gluten-free diet was just the latest celebrity diet fad but a lecture I recently attended by Dr. Peter Green, a world-class expert on Celiac disease and gluten-sensitivity, Director of The Celiac Disease Center at Columbia University and author of Celiac Disease: A Hidden Epidemic, convinced me otherwise. Celiac disease has been Dr. Green’s focus over the last 10 years with equal concentration on patient care and research. He is one of the few physicians in the United States with intense clinical and academic interest and expertise in celiac disease.
For years, the medical community believed that in order to have Celiac Disease, a patient had to have gastrointestinal symptoms. Research has shown the only 50% of patients report gastrointestinal symptoms such as diarrhea, bloating or gas. The most frequent symptom reported is fatigue. Other symptoms include muscle cramps, joint pain, tingling in limbs, mouth ulcers and irregular periods.
However, what wasn’t realized until the past twenty years, thanks to the work of Dr. Green and other top researchers, is that Celiac disease can occur in adults – the frequency is 1 in 133 people. The presentation of Celiac can be very different from person to person.
The symptoms for Celiac disease and gluten-sensitivity are different from those taught to most doctors, including me, in medical school. Celiac disease was mainly taught in Pediatrics as malabsorption syndrome, a disease where the intestine cannot absorb proper nutrients. Classic Celiac patients were shown as having rail-thin arms and legs and protruding bellies, but this is rarely seen anymore. Although diarrhea and abdominal pain account for 9% and 20%, respectively, of patients” symptoms, the scope of its symptoms is much broader.
The most common symptoms or medical findings are:
- Fatigue
- Anemia (low red blood cell count)
- Joint pain
- Headaches or Migraines
- Diarrhea
- Abdominal pain
Fatigue and anemia (having a low blood count of Hemoglobin) are common symptoms of Celiac disease in adults. Because the intestine is not absorbing nutrients properly, these patients become iron and B12 deficient. In this case, replacement therapy isn’t the answer because it wouldn’t address the underlying problem.
Women, especially those already diagnosed with Osteoporosis, should be checked for Celiac disease because taking medicine to strengthen the bones will only be a temporary fix if the real issue is poor intestinal absorption of nutrients. Dr. Green also made the point that undetected Celiac disease can lead to an increase in malignancies, such as Intestinal Lymphoma if left untreated. Low cholesterol and a low HDL can also be associated with Celiac disease – sometimes even a good thing, like low cholesterol, is too good to be true.
Eye Opening Case Study with Dr. Green
I discussed with Dr. Green a patient we both saw 20 years ago. She was seeing me for her asthma. However, she was telling me how tired she was and I drew blood her and found she was anemic. Her iron was low so I sent her to her internist who put her on iron pills. She didn’t get better after a few weeks and she came to me and said: “Do you think I could have Celiac disease?”
Truthfully, I had never seen an adult case in my first few years of private practice but I said we should check. I drew blood again and sure enough, she had positive antibodies that indicated Celiac disease. I referred her to Dr. Green’s Center at Columbia University Medical Center. She had an endoscopy that showed her intestinal lining had been damaged. She was immediately put on a strict gluten-free diet.
Then the mini-miracle happened: her energy came back. Her anemia resolved. Her joint pain went away!
Now I realized Celiac disease could masquerade as many other medical conditions.
Diagnosing Celiac Disease
The key lab tests Dr. Green mentioned to diagnose the Celiac disease:
- The screening blood test is the IgA tissue transglutaminase antibody (TTG).
- The conformational blood test is the Endomyosomal antibody (EMA).
Dr. Green still recommended anyone with the positive tests get an endoscopy to assess the intestinal damage.
There are many different ways to diagnose Celiac disease. The gold standard for diagnosis is a biopsy of the small intestine. This is done in order to detect the absence of microvilli, the finger-like projections that help increase surface area to absorb nutrients. However, before you even have to think about being “scoped”, there are blood tests available that indicate if you are a likely candidate for this procedure. The Tissue Transglutaminase IgA blood test is an excellent screening test to determine if a patient may have Celiac disease. A second blood test, called Endomyosomal antibody, will tell if a biopsy is needed. Another way to test for Celiac is through genetic testing. For this test, all the doctor has to do is swab the inside of your cheek and send it to the lab for analysis. If you have the genome HLA DQ2 or DQ8, you are at risk.
Celiac Disease Patient Case Study
Years ago, a young woman came to our office with multiple complaints. She had extreme fatigue, difficulty sleeping, overall body, and joint aches, and numbing and tingling in her arms and legs. She had seen multiple physicians, including a rheumatologist and neurologist. All studies were negative. She was told she might have fibromyalgia and given an antidepressant, which she refused to take.
This patient sounded like a patient with fibromyalgia and fatigue Syndrome. On further questioning, this patient also told us that she had a history of irregular periods and was told to take iron for anemia. And, after a careful review of all her prior studies and medical history, we began to suspect Celiac Disease, an autoimmune disease. An autoimmune disease is a disease where the immune system produces antibodies that attack the body. In Celiac Disease, the antibody is directed against gluten, which is a protein in grains.
This patient’s blood studies revealed an iron deficiency anemia, a B12 deficiency, and Celiac Disease. Her primary care physician told her that she couldn’t have the disease as she had no gastrointestinal symptoms. Lucky for her, she didn’t listen to him.
We explained the diagnosis to this patient and offered her two options: to go on a strict gluten-free diet immediately or to get an intestinal biopsy. As going gluten-free is both psychologically and physically challenging, the patient opted for the biopsy, which confirmed the diagnosis.
Going on a gluten-free diet, a regimen of B12 shots, iron supplementation, and other nutraceuticals resolved all of her symptoms. Her fatigue and sleep improved, her anemia resolved and for the first time in her life, her periods were regular.
What If I Don’t Have Celiac Disease Blood Antibodies, but I Think I Get Sick From Gluten?
Well, we discussed this as well. There is a medical diagnosis called Gluten Sensitivity (GS) and there are even more patients that have this than Celiac disease – it’s about 6% of the population.
Patients with GS have the same symptoms as a Celiac disease but without the positive blood tests and without the damage to the intestinal lining. Some of these patients do have a blood antibody called antigliadin antibody which can be positive in about 50% of patients.
How Can You Protect Yourself When Eating Out from Gluten?
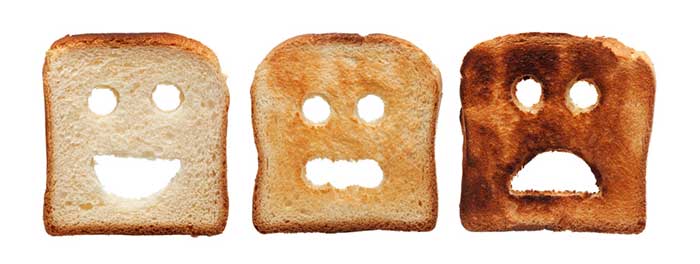
There is a great new device called Nima. It is a small triangular-shaped device that is very portable and can rest on a table-top. You can simply take a piece of food off your plate and place it into the device. Within seconds, the NIMA machine will either show a smile (very cute!) indicating no gluten, or a frown indicating gluten is present. This can be a huge stress reducer for those with Celiac disease that don’t want to accidentally ingest gluten.
Click here to check out the Nima device starter kit.
Gluten Freedom or Gluten Fear
We routinely screen many of our patients for Celiac Disease. However, even in those patients who test negative or “borderline,” we ask many of them to go gluten-free. Many patients report an improvement in symptoms within 4-6 weeks and sometimes sooner. Today, there are literally hundreds of gluten-free options at supermarkets and restaurants.
Many physicians are now realizing that some people without Celiac Disease respond well to gluten-free diets. Many of our patients come to us thinking that they are allergic to wheat. Wheat allergy is extremely rare, however, gluten intolerance is far more common. Therefore it is important to be tested prior to going gluten-free.
The take-home message is: there are different types of gluten/wheat intolerance. You can work with your doctor to get diagnosed and you need to trust your gut- literally!
I invite you to listen to the podcast to hear the full story from Dr. Green and myself and look forward to any comments on my Twitter handle @deanmitchellmd.
Listen to the podcast: Is Gluten the Number One Food Enemy?
Related Articles

- What is Candida Brain Fog and How Is It Treated?
- Could Gluten Sensitivity be Causing Your Chronic Fatigue
– Dr. Dean Mitchell, M.D.
Mitchell Medical Group, NYC
About the Author – Dr. Dean Mitchell, M.D.
Dr. Dean Mitchell, M.D. is a Board Certified Allergist and Immunologist based out of NYC. He graduated from the Sackler School of Medicine and completed training at the Robert Cooke Allergy Institute in New York City. He is also a Clinical Assistant Professor at Touro College of Osteopathic Medicine, a fellow of the American Academy of Allergy, Asthma, and Immunology, and the author of Dr. Dean Mitchell’s Allergy and Asthma Solution: The Ultimate Program for Reversing Your Symptoms One Drop at a Time. Dr. Dean Mitchell, M.D. has also been featured in The New York Times, The Huffington Post, Fitness Magazine, Dr. Oz and News NY 1. Dr. Mitchell also hosts the podcast The Smartest Doctor in the Room – a combination of a lively, personal and in-depth interview with top healthcare specialists.
This site contains affiliate links to products. We may receive a commission for purchases made through these links.
Reference
Non-celiac gluten sensitivity: All wheat attack is not celiac
Samuel O Igbinedion, Junaid Ansari, Anush Vasikaran, Felicity N Gavins, Paul Jordan, Moheb Boktor, Jonathan S Alexander
World J Gastroenterol. 2017 Oct 28; 23(40): 7201–7210. Published online 2017 Oct 28. DOI: 10.3748/wjg.v23.i40.7201
Ots M, Uibo O, Metsküla K, Uibo R, Salupere V: IgA-Antigliadin Antibodies in Patients with IgA Nephropathy: The Secondary Phenomenon? Am J Nephrol 1999;19:453-458. DOI: 10.1159/000013497
https://www.karger.com/Article/Abstract/13497#



