The End of Food Allergies – Is It Possible?
This post may contain affiliate links.
CONNECT WITH US:
Dr. Mitchell speaks with Dr. Kari Nadeau, Stanford’s top food allergy expert, about her new book: The End of Food Allergy, on The Smartest Doctor in the Room podcast. The discussion covers all the bases of preventing, diagnosing and treating food allergy.
Today, we are, again, going to discuss an important topic within the field of allergy. Food allergies. I have done several podcasts on this subject, but I just couldn’t pass up the opportunity to shed some more light on this disease when I found out my guest today, Dr. Kari Nadeau, just released her new book, The End of Food Allergies. She is one of the nation’s foremost experts in adult and pediatric allergy. I have to show this to my listeners and viewers. It’s also co-written with Sloan Barnett who is very interesting, her daughter suffered from food allergies.
Dr. Nadeau is the Naddisy Foundation Endowed Professor of Medicine and Pediatrics. And she’s the director of the Sean and Parker Center for Allergy and Asthma Research. Remember Sean Park from Facebook notoriety at Stanford University. She’s also the section chief in asthma analogy in the pulmonary allergy and critical care division at Stanford. I could go on and on. She’s got a lot of titles, which were really impressive. She is considered though, I will tell you this, for all the listeners, among her fellow allergists to probably be the most preeminent researcher clinician in the field today. And I don’t say that lightly. So when I was telling some other allergists that she was going to be on my podcast, they were super excited.
LISTEN TO THE PODCAST ON SPOTIFY
Majority of podcast conversation and main talking points below.
Dr. Mitchell:
On a personal note now, I actually met Dr. Nadeau probably over 10 years ago at one of the American Academy of allergy meetings in Anaheim, California. She was giving a lecture at that time on something very near and dear to me, sublingual immunotherapy. But I have to say this, and this is in all earnest, she is a hero, role model of mine in the field of allergy, and I’m going to explain. I too, as a lot of you viewers may know, I’m a board-certified allergist and I do podcasts on a lot of different subjects, but this allergy immunology infectious disease is actually my specialty.
But some of you may know that I had my own personal transformation in allergy back in 1998. I had switched my entire practice from allergy injections to sublingual drops. And I actually wrote the book myself, the Allergy and Asthma Solution, where I talked about my dramatic change in my career for various reasons. And it was quite controversial at the time and I felt quite lonely and sort of like an outlier, so that’s why it was really nice going to Dr. Nadeau’s lecture back then.
But I have to say something else. I also was not very proud of being called an allergist back then. I was actually slightly embarrassed when introducing myself to other doctors. And you ask why. Well, for good part of a hundred years, allergists were known as shot doctors and many colleagues seemed to mainly take pride in how many allergy shots they were giving in a day. Personally, I was dismayed at how the field did not advance since the days of the physicians that trained me. Many of them were trained in the fifties and they were doing the exact same techniques that I was being trained to do.

My guest today, Dr. Kari Nadeau is the polar opposite of your typical allergist immunologist as a researcher and a clinician. She is bold. She took the specialty of food allergy on with the mantra “failure is not an option.” And just to show her also, I still save the magazine from seven years ago when the New York times did a whole profile on her and what she was doing. I didn’t know we were going to have this interview seven years later, but as I said, truly, she was a hero.
And we know that trying to avoid a food allergy or multiple food allergies is not really realistic. Sometimes it’s almost impossible. So this book, The End of Food Allergies and her own personal research really is a testament to the fortitude to make children with food allergies and their parents have a better life. So after that long, a little bit winded introduction, it’s my great honor and pleasure to welcome Dr. Kari Nadeau to the podcast.
Dr. Nadeau:
Thank you so much. It’s an honor and privilege to be here Dr. Mitchell. I am so glad that we can reconnect through your amazing podcast that affects millions of people. And so I feel very lucky to be here today and I am so excited. And there’s so many people that have been in this field and I feel like we’re building on the blocks of so many talented individuals to be able to have the science that delivers on the hope and promise of therapy and prevention for many people that suffer from these diseases.
Prevalance of Food Allergies Now
Dr. Mitchell:
So Dr. Nadeau, it’s commonly accepted that over the past 30 years food allergies have exploded, really becoming an epidemic before we had this COVID epidemic. There’s clearly no hoax going on in food allergy. I have my opinions, which I’ve expressed a little bit before. 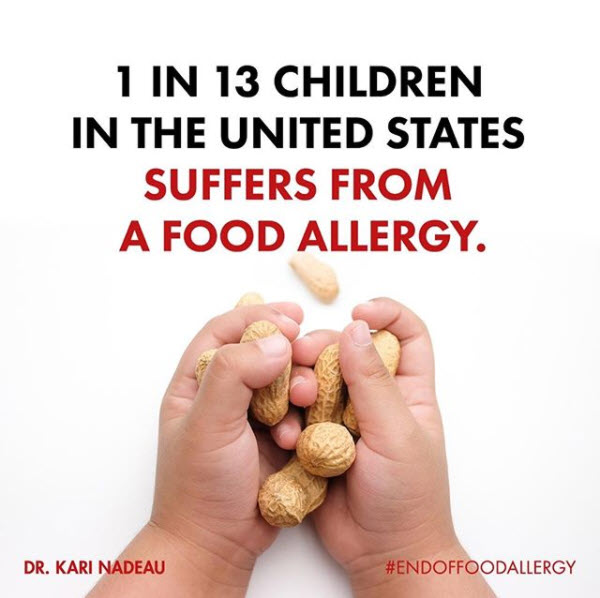 Why do you think we’re seeing such unprecedented number of cases of food allergies? And I should say, especially multiple food allergies. It’s not even like before you heard somebody had a peanut allergy. Now I’m seeing cases, I know you are, of children who have seven, eight serious food allergies. And I guess, obviously, we know it’s got to have some kind of environmental influence, it can’t just be genetic. So I know you talk about it in your book, which is interesting. So, but I’d like some of your pointers or observations on what you’re seeing out at Stanford.
Why do you think we’re seeing such unprecedented number of cases of food allergies? And I should say, especially multiple food allergies. It’s not even like before you heard somebody had a peanut allergy. Now I’m seeing cases, I know you are, of children who have seven, eight serious food allergies. And I guess, obviously, we know it’s got to have some kind of environmental influence, it can’t just be genetic. So I know you talk about it in your book, which is interesting. So, but I’d like some of your pointers or observations on what you’re seeing out at Stanford.
Dr. Nadeau:
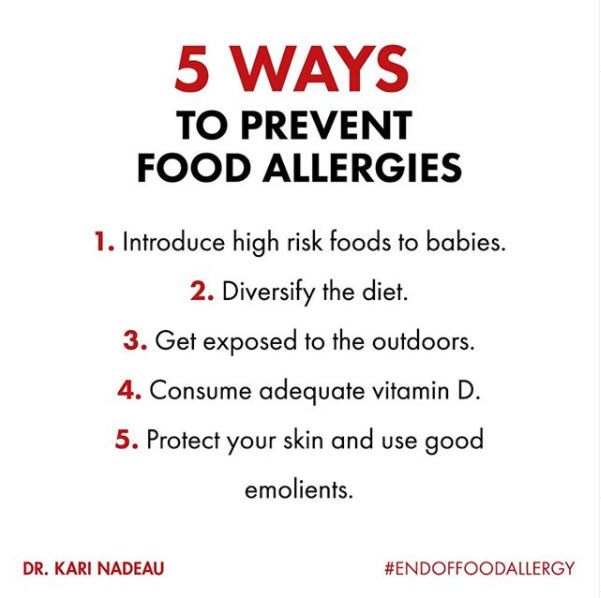
We’re really excited to be able to work with a lot of epidemiologists throughout the world that have published on some of these associations of what could increase the risk of food allergies. And we know so much more now than we did even 10 years ago, and even 20 years ago when I was training. And that science has now built up many strong facts that we talk about in the book, to be able to let someone who’s just delivered a baby or someone that might have a child already with food allergy, have a toolkit, have a how to list of how to prevent, because now that we know some of the causes, now we can think about how to change behaviors to prevent. So that’s all within the rubric of the fact that there’s about five Ds that we know potentially now lead to the increase in food allergy.

You’re absolutely right, Dr. Mitchell, there’s the fact that about 10% of now adults in the US have been diagnosed with food allergy, about 8% of children in the US have been diagnosed with food allergy. It’s not just the US anymore, in China they just released the data, about 8% of people in China have food allergies. So this was definitely growing throughout the globe, it’s just not in North America, it’s in South America as well.
Reducing Your Risk of Developing Food Allergies
To answer your question, we think some of the reasons is because back in 2000, a group of well-meaning people used a small amount of data to then make the guideline that they should avoid feeding children peanut, egg, milk, shrimp. And it turns out that that probably was not the best advice. It was based on the data that we had. But now 10 years forward, 20 years forward, we now have tons of data from thousands of individuals to say that diversity of diet is really important. So that’s the first D.
Dr. Mitchell:
I was learning things, reading your book, so yes. And I like to recommend it to my adult patients anyway, too. Don’t eat … That was actually one of the teachers, one of my really good allergy instructors, doctors, he was also a board certified dermatologist, he was a very bright guy, but he used to say, you don’t become allergic the first time you eat a food a lot of the cases, it’s always after repetitive eating it. So yeah, diversity of diet makes a lot of sense. I’m sorry, go ahead.
Dr. Nadeau:
Yes, no, no. It’s great. And then the immune system actually likes diversity of diet. So that simultaneously, if you can give all of the food proteins that typically are those that are associated with food allergies, now, like you said Dr. Mitchell, not only is it just peanuts anymore, it’s multiple. If you have one allergy when you’re an infant diagnosed perhaps by an allergist, you probably have a 45 to 50% chance of getting another allergy at some point in your life that’s food.
So we got to think about these, there’s a lot of cross reactivity in food allergens too, so I talk about that in the book. And most importantly this diversity of diet feeding, and actively we have to prevent allergies. Unfortunately, the way the environment is right now, we have to actively do something because tree nuts, for example, are doubling every 10 years. And a lot of adults are now getting food allergies that they otherwise were totally fine to eat when they were children.
So we’re understanding that diversity of diets is key, feeding something to babies early and often and regularly is very important, and starting with small doses even at four to six months of age is fine. That’s one thing we talk about. The other thing is dry skin. So you learned a lot about eczema, so did I, when we were in training, we know that eczema is related to allergies, but now there’s been even stronger evidence showing that if you have dry skin or eczema as a baby, you have a three times to four times higher likelihood of getting food allergy by the time you’re three. So taking care of dry skin’s really important. I talk about that.
Dr. Mitchell:
That’s really important. Yeah. For moms listening. Sure.
Dr. Nadeau:
So those are some of the causes. Vitamin D, having a good microbiome, having a dog in the first year of life, that also helps.
Dr. Mitchell:
Right. That really throws people off because I’m sure … Also, again, I see in my private practice, I have my practice on immunotherapies on treating dog and cat allergies. Actually, I’ve treated a couple of veterinarians also. It was unbelievable. But yeah, and so when you tell a family, yes, you should have a dog early on, they’re like what?
Dr. Nadeau:
Right. But not when they’re allergic. Exactly. So we did talk about all these things.
Dr. Mitchell:
Yeah. Okay. But the thing … I’m going to bring up a couple of … You brought up some really important things, and I’m going to tell you what I saw in my own clinical practice. Obviously, I was following the literature, but I had a couple of traumatic cases too. I’ll just say I have not forgotten in the last year where I had parents who came in with their twenty-something old children that had multiple food allergies. And one of the things that came up was because they had other children that did not have food allergies. And in two of the cases, the moms had gotten antibiotics during the pregnancy, because they had to, there was an infection and had to be treated. And I’ve also seen, I know there’s been reports, I think he’s published in the past. That a lot of times when these kids are getting a lot of antibiotics for ear infections, throat infections, it’s changing the microbiome. Do you think … we know, you mentioned the book The Hygiene Hypothesis for those who are listening about avoiding, being more… It’s too clean an environment and all those things, I think, as you say, in the books, it’s falling by the wayside. But I think antibiotics, and obviously got into the food supply may have been a dramatic microbiome disruptor.
Dr. Nadeau:
I absolutely agree with you. And we want to, talk about in the book, all the possible science that has led to the deterioration of a normal gut, the disfiguration of just normal healths. And why we’re getting so many allergies, we talk about detergents and how that might be changing the skin barrier, not just on the top of our skin, but also in our lungs and in our gut. But like you said, what about antibiotics? And there is an association that is tenable and there are many trends to show that if you do use a lot of antibiotics, your gut is not happy.
It can in some people be irreversible. And we need to think about the overuse of antibiotics and how that changes our gut. Because my colleague, Justin Sonnenburg at Stanford, and David Relman have shown that if you don’t have good microbiome and fiber and healthy vegetables and healthy fruit, that you lose this beautiful mucosal lining inside your gut. And when you lose that, you’re much more apt to get GI like diseases, like food allergy. So I think there’s definitely something there. I think the Hygiene Hypothesis is important because there are viruses that can stimulate allergies, but then there are bacteria that can help improve it. So there’s always a balance of any of these particular thoughts about what’s causing allergy, but at least in the book, we do talk about the strong facts and how to behave differently.
Dr. Mitchell:
Absolutely. I like also what you’re talking about, the topical. Again, I’ve heard it before. I think Hugh Sampson has brought this up. It’s interesting people don’t realize so many baby products, from the shampoos to the soaps, they probably had different types of nut base oils in them. And again, you’re right, the predisposed child that has dry skin or eczema, those seep in through the skin. And cause, as we know, pomology and our training, the skin is one of the top ways to sensitize, it makes somebody allergic. In research labs, when they try to make mice allergic, they put patches of penicillin on there.
Dr. Nadeau:
That’s exactly right. You and I read that wonderful article by Jonathan Spergel and Reif Geha, showing that if you excoriated scraps the top of a mouse’s back and then laid peanut oil in, like Hugh Sampson had mentioned, that will activate a peanut allergy and that’s what we do. So, I think there’s something there, I think we have to be more and more careful how to protect the skin. Absolutely.
Recommendations for Families with Kids with Food Allergies
Dr. Mitchell:
Those are great points. I think for anyone listening and we’re going to get more in depth about the early introduction of foods in a few minutes. But again, people listening, I think hopefully going to learn a lot.
Let’s turn to something which I’m so glad you addressed. You’re an exceptional physician researcher because a lot of doctors like to just look at the technical type of things, and the biology, and the pathology. But you talk about in your book, and it was one of the things that really struck me in the New York Times article about you, how you get so involved with the families. And I want to talk about the psychological, emotional toll on families, which is not always appreciated. I’ve personally known, because my sons who are now in their 20’s and one’s 30. They both had friends that had severe food allergies. And we knew the parents. And I always joke around the parents used to like when their kids had sleepovers at my house, because I’m an allergist.
Dr. Nadeau:
Exactly, they’re safe.
Dr. Mitchell:
I should know how to use an EpiPen.
Dr. Nadeau:
Exactly.
Dr. Mitchell:
But you would see what these families went through. The kids had to be more resilient. The parents, and the moms especially, were on pins and needles all the time. So I know you’ve seen hundreds of food allergy families. What is your approach and how do you advise them? Again, you’re seeing a new family and they’re afraid. What kind of either counseling, groups support, what do you recommend to them? I’m just curious.
Dr. Nadeau:
Well, first of all, thank you for mentioning it. I can tell that you are also a compassionate doctor that cares about these other aspects because when we take care of anyone with allergy, anyone that has them we take care of the whole person, and the whole family. And as Allergists we have this, I think incredible accountability and responsibility, as well as privilege the fact that we take care of all ages.
Dr. Mitchell:
Right? People always asked me why I went to allergy, I’m so sorry I have to bring this up for a second. Because people would ask me a lot of times, why did you go into allergy? And I would think for a second, it was a gut reaction. I said, when I trained in internal medicine during the AIDS epidemic and that was unbelievable. But I said, when I got out of that training, I really missed taking care of kids and adults. I didn’t want to be pin holed into one area. And in allergies to, it has the immunology background. I probably would have been a family practitioner if I didn’t do this. So anyway, yeah. So it is, we’re so fortunate that we get to take care of families, because this runs in families. Anyway, sorry.
Dr. Nadeau:
And that’s … what I always want to do is see how the family’s reacting. And it’s a team approach, it’s not just about me. I think the children and the families, like you said, and the patients with food allergies that have been suffering it through so much of their life. They’re the real heroes. They’re so courageous and I’m glad that FARE and other nonprofit organizations see that and understand that as really reaching out to be advocates for families and voices. So, oftentimes I approach it to understand where are they coming from, are they just newly diagnosed, let’s make sure we get the diagnosis right. I … very open to discussions.
There are so many different diagnostic tool sets out there. Some of them are not so helpful. Some of them are helpful. So oftentimes the first time I meet families, that’s a lot of detective work as to if they really do have an allergy or not. As you know, using our tried and true skin tests, blood tests, and then a food challenge if we need to. But importantly, it’s a discussion, it’s teamwork, it’s going both ways between myself, and the parents and the child, if there is a child or the patient and myself if it’s an adult.
But to me, it’s a process of making sure that we develop a good rapport. And then also making sure that I can talk about some hope and promise about therapies, if they’re interested in talking about that. No matter what though, when we do talk about it, every person has situational anxiety as they should. They talk about their worries. It’s a disabling disease. We talk about food labeling. We talk about a lot of things that are in the book, but that anxiety is real. We need to take food allergy seriously and to make sure that people carry an injectable epinephrine device, but know that this is a life long discussion, that this is teamwork and a relationship that will build for a long time. And that’s part of the reason, like you said, we go into allergies because we’ll follow these patients long-term to make sure we can manage them well.
Dr. Mitchell:
I have to tell you a story of mine, because you never forget these things. My first patient in private practice, literally the first patient, a pediatrician referred her to me, I had just opened up my practice. I was sitting around all day, wasn’t seeing a lot of patients. It was my first patient, it was this little boy, cutest little boy, who was actually from Guyana, his family. And very tiny, he was so tiny and he had severe peanut allergy. And his mom used to bring him in to me and he also had environmental allergies, which I took care of at the time. And she used to come to me, Dr. Mitchell, she goes, promise me my son’s not going to die, so that was one thing we’re dealing with. The other sad thing, which has really changed, thanks to you and as you mentioned, FARE. When I used to … break my heart and this is, you’re going back to 19 … 1991 or so, he used to when he would go to school, he had to sit … He used to have to his lunch in the library.
He used to have to sit aside from everybody else, he was essentially being a loner. And what I gave this boy credit because he wasn’t really … he had a great mom, like a lot of these food allergy moms. Just luckily born into the right family, and she was so supportive of him. And he ended up growing as I said from this tiny little boy to this six foot three, because I ended up seeing him years later. I used to pick him up with one arm, he could lift me up now with one arm, and he got through. But as I said, I remember the difficulty for him. And I know that things did change. Again from FARE and other things that they made more … they work with schools to make … help kids not feel so separate or different. And so, but do you … I guess you probably encourage, I know a lot of the families do on their own, to get on these support groups to join because that’s where they had to talk to other moms that are going through the same thing.
Dr. Nadeau:
 Exactly. Other parents, other caretakers and other of the teenager summit that the FARE has. A lot of the adolescents that are suffering from this. It’s great to talk to your own group. I feel so lucky that for the book we’ve put out, a website, we have a Facebook site, an Instagram. I’m really pleased to see the blogs that are now happening. And then what I’ve been, I think very privileged and with the book I’ve been able to go on different Facebook groups and talk to moms and parents and dads. And you see that this is an issue that’s not just around my clinics. These are very common questions that you get all over the world. And you’ve probably seen that too, Dr. Mitchell with the fact that there are some unanswered questions, and we’re very careful in the book to explain what things we know and what things we don’t know. There are a lot of myths out there that we need to just bust down, because we have enough science now to say, no, that’s not the way to diagnosis. Or that’s not the way treat this.
Exactly. Other parents, other caretakers and other of the teenager summit that the FARE has. A lot of the adolescents that are suffering from this. It’s great to talk to your own group. I feel so lucky that for the book we’ve put out, a website, we have a Facebook site, an Instagram. I’m really pleased to see the blogs that are now happening. And then what I’ve been, I think very privileged and with the book I’ve been able to go on different Facebook groups and talk to moms and parents and dads. And you see that this is an issue that’s not just around my clinics. These are very common questions that you get all over the world. And you’ve probably seen that too, Dr. Mitchell with the fact that there are some unanswered questions, and we’re very careful in the book to explain what things we know and what things we don’t know. There are a lot of myths out there that we need to just bust down, because we have enough science now to say, no, that’s not the way to diagnosis. Or that’s not the way treat this.
Tips for Preventing Food Allergies in Kids
Dr. Mitchell:
Right. It’s so important you bring that up. I’m just going to interrupt for one second again, which I unfortunately interrupt a lot. But prior to a book like yours, and I think hopefully like mine. I was always also very careful in my title. They originally wanted me to write The Allergy Cure, which I didn’t want. Because you can go to … back in the day when people went to bookstores, and see a whole shelf full of books saying the allergy cure, dah, dah, dah, dah, all these false promises, not reliable, explaining the testing. So a book like yours really is the go-to type of book for a parent, especially if they first hit with this. And they need to know what is real, what is not, where do I get my bearings to start exploring what my options are?
I’d like to move into about early intervention as you were touching on before. Many of our listeners who have a child with food allergies, certainly, probably they’ve heard about the recent change in the approach to preventing food allergies. The LEAP study, which stands for the learning early about peanut allergy, I think jolted allergists more than anything to change the classic advice to avoid foods in early childhood. And we did a complete 360 and we said, oh, start having those foods by four months of age. And again, you can understand this, there are parents that are like, what? I’m petrified, I have an older son that’s peanut allergic and I’m going to start feeding my younger one peanut?
 So I want to ask you, because we’re going to bring up some things here. But how do you find, do we proactively and practically get this out to, especially pediatricians who are taking care of these patients. A lot of times their not even at an Allergist’s office yet, so that they become aware. How are you working at Stanford, maybe with the other doctors there, getting the word out that … advise your moms and families to get these foods in early?
So I want to ask you, because we’re going to bring up some things here. But how do you find, do we proactively and practically get this out to, especially pediatricians who are taking care of these patients. A lot of times their not even at an Allergist’s office yet, so that they become aware. How are you working at Stanford, maybe with the other doctors there, getting the word out that … advise your moms and families to get these foods in early?
Dr. Nadeau:
Excellent question. I‘m so glad you’re bringing it up because it is counter to what we had learned 20 years ago. And again, like I said, the well meaning group of people work with a very small amount of data. What was happening was, unfortunately we see small blips of rises of food allergy in the 1940s. Then in 1960s a little bit more. Then in 2000 they put up those guidelines. Well-meaning individuals in the year 2000, the American Academy of Pediatrics said, okay, avoid all those foods. Then after the year 2000 it went up like this.
And so then we realized, wait, that might not have been a good idea. So I think again, I hope that the pediatricians, that the allergists know that right now we have so much data. That it is true, that if you diversify the diet early and often, that does prevent, that has shown reproducibly now in Europe, in Japan, in Israel, in the United Kingdom, that all of this really helps. And so I think that we are in a new paradigm. I think that we need to embrace it and help babies reduce the likelihood of food allergy because this epidemic is going too fast. We won’t be able to treat everyone. So we need to prevent.
Dr. Mitchell:
You know, it’s interesting you bring up about the different countries. And I want to share a story for the listeners. It’s interesting, I did training in Israel and the story that really was dramatic that I’ve read in a lot of lay articles was actually about the story about Gideon Lack, the London allergist, and it’s so interesting. He was invited to speak in Israel and he’s a well-known allergist in London. And he typically says that when he would give lectures, he used to ask the allergists in the audience, how many of you have patients among the pediatricians that have food allergies. And when he would do it in London, a lot of hands would go up, when he came to New York, a lot of hands went up and went to Israel and like one or two hands went up and he said, “Hmm, what’s going on here?” And then he decided to do a study where he actually, I think he looked at the Jewish population between those three countries and he saw that there was a dramatic difference.
And again, he got the aha moment when he was talking, I guess, to the Israeli mothers, pediatricians, that they were all eating this snack called Bamba. We’re eating Cheerios, they’re eating this thing that’s got like Sesame seed and peanut in it. And he said, could that be the factor? And just so far to know, so that’s where the science came from. I want to ask your opinion. I don’t know if you’ve been recommending this or not, I was watching one of my favorite shows I used to get to watch a lot was Shark Tank. And one day I was watching it on a Friday night and there was this company called Ready, Set, Go. And they’ve come up with a powder, which I think is a mixture of peanut, milk, egg, the common food allergies, trying to make it easier for parents. So they’re not busy measuring out the amounts. What do you think about that?
Dr. Nadeau:
These stories are so important to explain how discoveries are made and to make sure that yeah.
So, we learned right away at Stanford and Gideon was a good colleague that I didn’t want to just think about preventing peanut. I wanted to prevent everything. I was treating multiple food allergies. So I had parents that were having children that those babies were not food allergic yet, but they always were asking me, what should I do now? And as a protein chemist, I knew that you should be able to prevent any food, not just peanut, but if you put it into the food item for that infant early and often, it should be able to prevent that specific food allergy.
That’s exactly what we did. We mixed shrimp, milk, egg, wheat, tree nuts, peanut, soy, Sesame. And we included others as well, because I thought let’s just pack it all in there. And initially we did it through powders at Stanford, and then we patented it. And then once we patented it, Stanford said, “Let’s go create a company.” And, and I decided that instead of just doing three at a time or two at a time, let’s make it easy. Let’s do all 16 to be able to prevent. And so we started a company called SpoonfulOne.
We are so happy that it’s working so well, it’s very safe. So yes, there is this opportunity between around four to six months of age to start doing mixtures of foods. And I would recommend that for anyone that doesn’t have an already doctors diagnosis.
We have puffs and crackers. And then also we have a packet of all 16 food proteins, and they have high integrity. We actually treat it as if it was … because it is going into infants. We make sure that there’s no other issues with it. So we’re so excited about it and yes, there are other companies moving forward as well. Like the one that you mentioned. I’m getting 16 foods done at once.
Diagnostic Food Allergy Testing
Dr. Mitchell:
No, it’s smart. It really is. I mean, why not? Okay. Let’s move on to diagnostic testing. This is going to be something interesting now, too, we’re going to talk about, and as I said, this is going to … we’re going to get into very specific things. As I mentioned how I was always a little bit dismayed about allergists, not really changing or advancing from practices a hundred years ago. And we all know that allergists for really a hundred years, skin testing has been quote “The gold standard” or whatever. And it hasn’t changed much since the days of, I think, Noon and Freeman over in England, in 1911. But, we know that laboratory testing is getting more interesting. I like to use a lot in my practice, something called Component testing, which I’m sure you’re aware of.
I think it really gives you the specific things that obviously without the risk of testing kids. So my question is this, so it’s going to be get I know you’re an academic and everything, but my question is regarding the gold standard of food allergy testing, the oral food challenge, is it still the only option to confirm a diagnosis of food allergy? And I want to ask this just with the two caveats, especially in the light of COVID-19, it was just actually an article in the journal of allergy this in practice this month about that. And it also brings up a little bit of Mary Lovelace. No, because just so I have to share with the audience, because I did see one patient, believe it or not in my career that saw Dr. Lovelace. And this woman was terrified of going to a doctor, because as a child, they brought her there and just for the listeners to know back what they did then, as I said, I give Dr. Lovelace a lot of credit.
She was the expert on the venom, which gave a lot of credibility to the field of allergy, but she had a sting room. They used to bring the kids in. We’d get used to get stung by the bee to see that if they had, if the immunotherapy in the other shots had worked. So I sometimes feel, I hate to say this, that the oral food challenge is a little bit of the sting room brought in. So can we rely on some blood testing? You know, there was also an article, one of the recent journals about, and things that I want to start looking at, because I’m starting to do I’ll to you about some food allergy treatment that like the basophil activation test or a specific IgG4. Can you talk a little bit about that? I mean, because also too doing food challenges is really for really specialized practices. It’s not for the routine practices that we see.
Dr. Nadeau:
I agree with you, Dr. Mitchell, the food challenges are draconian and we create so much anxiety in doing them. On one hand, I understand that the FDA needs that defined very specialized and that probably won’t change for a while, but we can create the change and we should. We have to push the science to do better because I feel for that patient and that mother and that father who just come into the office kind of trembling even when the skin test is negative.
It’s hard. So, I feel for my patients and that’s, what’s inspires us to get better at our science. I really believe in community-based participation that our patients should be the ones that say, wait a minute, why do we need to do it to do a food challenge? So there was a great paper by my colleagues in Boston, Lynda Schneider and Andrew MacGinnitie. And then Scott Sicherer at Mount Sinai also published a paper with Bob Woods showing that if you have a political history and you have a certain threshold of a component, let’s say Ara h 2
And when you have a certain skin test positivity. There’s a nomogram that you can just pretty much show that, okay, you’re going to get a positive food test result. So if you just line up the ruler and it’s over 95%, just don’t do the food challenge. So Lynda Schneider and Andrew MacGinnitie published a beautiful paper in which hopefully all of your listeners, I’m happy to share it with people. It shows that about 50% of food challenges are probably unnecessary. You could have probably just figured it out using the blood tests and the skin prick tests and clinical history, importantly, and that’s why you got to go to a board-certified allergist. You can’t just sort of look at a sheet because if you look at the sheet for blood tests, as you know, the computer will just say high, high, high, high, high, and that’s not necessarily true.
You need someone who’s experienced interpreter.
Dr. Nadeau:
So with that, I agree with you. There is going to be an age and oh, it hopefully you’ll write the book, the end of food challenges because we need that. We need to do something better. We need to get rid of this draconian practice. But right now it’s our practice to be able to have an end point for an FDA approved drug. And I really also talk about in the book that we need more FDA approved drugs. We need more choices for patients for multiple food allergies as well. So this is the beginning of the end of food allergy. We have PALFROZIA. Fantastic. Now let’s move forward.
Food Allergy Treatment
Dr. Mitchell:
We’re going to get into those in a second. Yeah. I don’t want to give away too much of our inches up. So those are great points. Okay. Let’s move on to treatment too because I’m sure this is what everybody really tunes in on for, and when we get into the end of the food allergy. So for decades, once a family realized that their child was food allergic, the only option for long time parents and the children were told, was avoidance. And sensible, yes, except practical, not really. Especially when the number of food allergies increased in so many of these children, it really became almost impossible. So I want to ask you obviously being at the forefront of so many research protocols over the years, and you talk about this in the book, which is really good.
I mean again, so helpful to the families going through this. No we really have about, I would say two options right now, but maybe three on the, well … some variations, there’s the oral immunotherapy, which you talk about. And I know you have this tremendous experience with is the sublingual immunotherapy, which again, I know you’ve done work on, I’m doing that now. I’ve worked with Edward Kim a little bit on that. I’d like to talk about that a little bit. And there’s of course the what’s called the epicutaneous immunotherapy, the patches.
So if you could explain for our listeners a little bit about each one and a little bit, I guess your pros and cons, because that’s why we might debate a little bit. I want to hear, I enjoy hearing from you and I’ve talked to Edward Kim and Anna. We all have our … but you can have tremendous experience. You’ve been through all the trials with patients and we’ll even actually toss in a little bit about maybe even the monoclonal antibodies, their role in this and you can mention about PALFROZIA so please tell us a little bit again.
Dr. Nadeau:
Yeah. And I know that you have the same goals. We want the best choices for our patients and one size doesn’t fit all. That by having choices we also need to make sure we understand as doctors, which patients will be enabled by this therapy the best. And we have some patients that don’t want to touch the food. They don’t want to eat the food. That’s where the patch of some liberal might be way better. And so I think that I having FDA approved drugs, I pick epicutaneous, sublingual immunotherapy, as well as oral immunotherapy. And then the biologics that you can talk about. These are the choices we need. When we think about cancer therapy, we have our first drug ever approved by the FDA. That’s incredible. That was last year. And that’s why I wrote the book to make sure people know that, okay, the train is moving, let’s get on it.
But so to answer your questions, oral immunotherapy, it’s got to be carefully done. It’s got to be done in a clinic with a board certified allergist who knows what they’re doing. You just dose very slowly and carefully, and you increase the dose ever so slightly every two weeks. And that builds up the immune muscle so that you can get rid of the allergy eventually, but it takes a long time. And you’re basically changing your threshold for you so you don’t have to worry about an accidental ingestion and for a lot of people that’s fine.
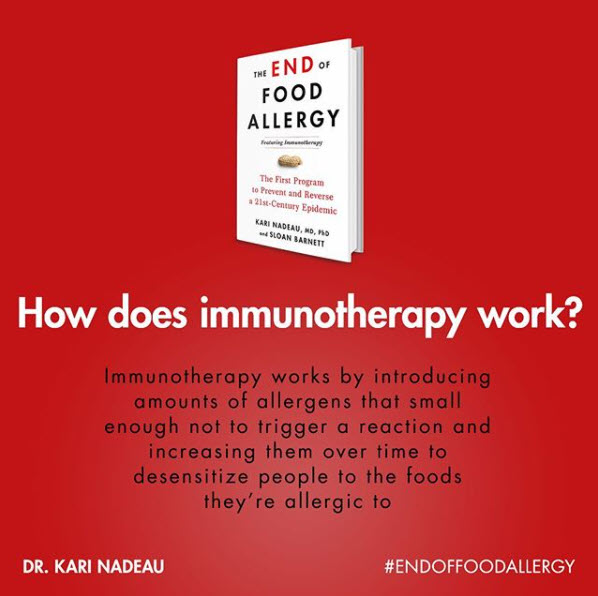 But while you’re doing this, while you’re training your immune system and building your immune muscle, you can have reactions along the way. And during immunotherapy, that’s more common than let’s say the epicutaneous, this patch or the sublingual immunotherapy, which is a much smaller amount. And there are reasons why for each of these because the gut is automatically tolerant. It’s very helpful to eat it. And because you have these special immune cells in the gut that take up the food and then become tolerant, but people don’t necessarily like to eat the same thing that they were allergic to.
But while you’re doing this, while you’re training your immune system and building your immune muscle, you can have reactions along the way. And during immunotherapy, that’s more common than let’s say the epicutaneous, this patch or the sublingual immunotherapy, which is a much smaller amount. And there are reasons why for each of these because the gut is automatically tolerant. It’s very helpful to eat it. And because you have these special immune cells in the gut that take up the food and then become tolerant, but people don’t necessarily like to eat the same thing that they were allergic to.
Right. I’m excited about PALFORZIA and I really believe in the data, the fact that they could get 87% in their active arm and only 4% in the placebo arm, we know that it works. The issue is how can we make sure it’s safer and even works better. And that I do use the four-letter word cure. Like how do we get to a cure? How do we stop it and make sure that people are going to do well. So these assays that you mentioned, the skin prick test, the Component testing, the basophil assay. All of those, not only can they be used for diagnostics, but they can also be used for.
Dr. Mitchell:
I’m really excited about it. Yes, that’s what I’m searching because you know, I’m doing the sublingual immunotherapy now, and I know it’s a lower dose, but the data is really good.
You know, at the end people are… Of course the patients always ask me, how do I know I’m better? I am like, “well, you’ll see in the real world if you do okay.” But it would be so nice to have a basic full activation test. Or I like to look at… even when my immunotherapy patients who are environmental allergies, I treat them for animal allergies…
I check this specific IgE 4 so when I see there are certain high levels and I have a better conference because I see… They’ll tell me that before I couldn’t walk into a room with a cat and now I can be with it a few hours. Yeah.
And that’s key. That’s what’s exciting and we talked about that in the book, let’s have choices for patients, and this is not for everyone, but when you need to talk to people you talk to your team, and the sublingual immunotherapy. There’s a lot of good data out there. And even though head to head, it didn’t do as well. So no matter what, each patient is different. Those clinical trials do not mean that it didn’t work. It means that it can be working in different circumstances.
Dr. Mitchell:
We also know too, our goal as allergists and the doctors and the community is to really make… To ease that burden, that fear, you know what I mean? If I can treat a patient, that they know they can go to a restaurant with a friend and not worry that there’s a peanut or a walnut or something in their salad, and then they’re off to the emergency room and they get that protection. That, to me, is a victory.
Dr. Nadeau:
Absolutely. Totally agree. So each person deserves that chance.
Advances in Food Allergy Treatment
Dr. Mitchell:
Yeah. Can I ask you a question too? ‘Cause I was asking Edwin Kim about this also, so age wise… I think there’s a couple of factors with immunotherapy to which you bring up, it was really great. It was at the end of the chapter. It was like a checklist. I also give such careful consideration to a child’s age. I give consideration to their parental situation. I mean, sometimes it’s very difficult to divorce. Family has to go back and forth. Are they going to be watched? Are parents both working? So I wonder also when you do… I mean, do you also sometimes wait until about four or five years old? Because some of these kids do have strong allergies, but to maybe see if they grow out of it or again, we want the child to be a little more compliant and be active.
Dr. Nadeau:
We need to make sure that this is compatible and if someone’s going to have reactions, even though they’re mild for the most part, we want to make sure that the parents are connected and that people aren’t going to have mistakes in the dosing and that there’s not a lot of room for error and that people carry an injectable epinephrine device at all times during this therapy.
There’s a lot of hope and promise here, but it’s got to be done just like most therapy, right? There’s always some guard rails around it. So that’s important.
Dr. Mitchell:
Sometimes to really judge the parents. It doesn’t matter their socioeconomic background. It seems like there are a lot of… I mean, some of these children are so lucky to be born to the right mom or dad, and I’ve seen… Sometimes people who come from poor backgrounds that it’s really hard, but the mothers are fantastic and if I think they’re going to be good about it, I’m like, “okay let’s do this.”
But if it’s another one where they say, “Oh, I can’t remember the dosing and this is too hard” then I’m like, “this is not for you.”
Dr. Nadeau:
That’s right. It’s got to be done with the right people and the motivation and the preparedness.
And you’ve got to get a good sense of that. Or if something changes while people are taking immunotherapy, like what we do in clinical trials, we understand things are tough, especially with COVID. We get that and we do need to have more telehealth visits and more accessibility and I’m so glad that the FDA and the NIH, they’ve been holding our elbows during this whole crisis to be able to continue to do food allergy clinical trials to continue to help food allergy therapy, but do it carefully in the time of COVID.
Dr. Mitchell:
Where do you think… We just briefly mentioned about it. I don’t like to use it a lot personally, the monoclonal antibodies for asthma. I usually find I can do without them. But it was interesting because I think Xolair, I forgot the generic name for it, was originally for food allergies and apparently it didn’t really cut the mustard, but it seems like it’s kind of like in the example… It’s like in the military, you have your air power overseeing so the ground forces can go in. Do you think that there are cases where if you were in practice that you were… You mentioned actually, I think it was with Sloan Barnett’s child, that they did Xolair on top of while the desensitization was going on. What’s your thoughts on how often that should be done? Because, again, it’s hard getting the drug companies… I mean, there’s companies paying for all of this. And they’re like, “well, we’re paying this for this and this or this, you know, pick one,” right?
Dr. Nadeau:
For private allergists too. I talk about that in the book. Like, what are the things that are some options right now? And I understand there’s a lot of discussion in our conferences about using oral immunotherapy.
There is a phase three trial right now. Thank goodness. I actually was down on that working with Genentech together on breakthrough therapy, designation with the FDA, with the NIH and Novartis, and we have a special group at the NIH that’s doing food allergy research. Edwin Kim is a part of it, so is Anya. It’s called the coFAR. And so with that, we showed that the multiple food allergy therapy with Xolair could be done safer with Xolair, and that’s been proven and published. You’re right. Xolair doesn’t work perfectly for everybody, but for the majority of people, it really did protect.
Now I understand it’s a biologic. We want to make sure it’s covered by insurance. Like you said, we want to make sure that everything is accessible for people and that’s why FDA approval is so important. And we want to help multiple food allergies too. So there is a phase three… For all of your listeners to know, a phase three trial means that that’s the step right before an FDA approval. So I want to let everyone know the time is now, the time is coming, we are working really hard. You can go on the website and if you do have multiple food allergies, there’s a clinical trial right now accepting patients to come in, to use Xolair plus multiple foods.
But as for how it works, Dr. Mitchell, in terms of getting Xolair for people, I always tell people if they want to try it, they can, but that there is a possibility without Xolair and there are other biologics coming up. That’s going to be very exciting. There’s Anti-IL-33, which we tested last year. That’s exciting. There’s vaccines and then we actually just created a company called Hygienics that inhibits each different, what we call, peptide or component as well. And then there’s another company that’s making all the food allergens at once to desensitize to. So there’s a lot of excitement around this.
Dr. Mitchell:
Oh wow. I think the other good thing too, even with the monoclonal antibodies, like Xolair, hopefully it’s not a lifelong thing. Sometimes when people would ask, “I don’t have to be on for many, many years,” this would be obviously a transient period until they would have properly desensitize and then you could pull that out.
We’re going to go onto something else. We’re getting near the end. But there’s something else that, which also a lot of allergists, we don’t talk about this. You wear a lot of different hats. You guys sold all your directorships, which is amazing. But to be honest, I don’t think a lot of people are aware that allergy training programs will come. In the country they are being eliminated and the positions decreased. I know my program, the oldest program I think, in the country at the Cooke Institute, was disbanded a little over 15 years ago. Pretty sad. Where do you think the future allergy doctors are going to come from and how can current allergists become proficient in some of these newer techniques? What’s your feeling and what you’re dealing, I’m sure, in the Stanford area when you’re dealing with people in private practice? Because not everybody unfortunately has the option of coming out to Stanford or sometimes coming to New York to Mount Sinai to get in and get into these trials. They want to see their local allergist or whatever.
Dr. Nadeau:
I think FDA approval is going to help make sure this gets out there for all of our fellow allergists. And they work so hard and they spend long hours. And of course, with COVID it made it even harder. And we work in diseases that produce a lot of mucus and that mucus, it’s definitely more difficult when you have viruses, eczema, and asthma too. So we’re really on the front lines a lot of times, and we are the go-to people. I understand that and that’s a privileged position. And in that I am hoping that by having more therapies available, that allergists can get trained more on how to use these therapists when there’s a training program. But I agree with you. I am also very saddened when training programs are shut down and we need to make sure that more people are going into our specialty because one in three individuals on the planet has an allergy.
And when we have science to back us up, which we do, and we have better therapies now, moving forward, and many more companies are now working in the allergy space. When we have the opportunity to fix these diseases like drug allergy, insect allergy… You write so well in your book about some of the immunotherapy and dog and cat and environmental allergies. These, I call, the Ruby slippers are in our hands, right? We have some answers here. We need to be able to get more trainees out there to clinics so that we can help people. For example, in the Bay area, it takes nine months to see an allergist. Nine months.
We need more people and we need more allergists. I hope that we inspire some people to train in our wonderful field.
Dr. Mitchell:
You know what I think too? I mean, again, that’s why I think you’re special and there’s other people out there too. I tried to give lectures before this whole COVID thing. It’s also about education. It’s like, you can’t be just cooped up in your office. I mean, you have to get out there. I used to always love doing grand rounds or speaking to doctors. It’s fun. You really get to speak with your colleagues and really exchange information and honestly a lot of my listeners know the reason I do this podcast. Obviously it’s a lot of selfish, personal, fun. I get to talk to top people in so many different areas of medicine I’ve always been interested in and learn what they have to say, because when we stop… I was telling my students, I teach at the medical school in New York, when you stop learning, you’re finished, hang it up.
Dr. Nadeau:
And that curiosity, that’s why it’s so great that you have this podcast. I’m so grateful. And that’s exactly right. That curiosity is key and we’ve got to inspire people and educate and that’s part of the book. I hope people like it. It’s also on audible. So that’s fine.
Dr. Mitchell:
Oh wow, that’s crazy. You can listen to it while you’re driving. So again, it’s The End Of Food Allerggy by Dr. Kari Nadeau, allergist extraordinaire out at Stanford. Just as I said, I love this book. I actually have a couple of copies that are going up from my office and hopefully encourage my patients to get it, who want to find out more. Thank you, Dr. Nadeau for coming on and taking the time to be here.
Dr. Nadeau:
It’s a pleasure and an honor. Thank you for your time today.
I think the end is coming at some point, but I’m so glad and thank you for having me on your show today. Really appreciate it. Have a great day.
Dr. Mitchell:
Thank you for listening to The Smartest Doctor In The Room with host Dr. Dean Mitchell. You can continue this conversation on Instagram at @deanmitchellmd, Facebook at Mitchell Medical Group or at deanmitchellmd.com.
About the Author – Dr. Dean Mitchell, M.D.
Dr. Dean Mitchell M.D. is a Board-Certified and Immunologist based out of NYC. He graduated from the Sackler School of Medicine and completed training at the Robert Cooke Allergy Institute in New York City. He is also a Professor of Clinical Immunology at Touro College of Osteopathic Medicine, a fellow of the American Academy of Allergy, Asthma and Immunology, and the author of Allergy and Asthma Solution: The Ultimate Program for Reversing Your Symptoms One Drop at a Time. Dr. Dean Mitchell, M.D. has also been featured in The New York Times, The Huffington Post, Fitness Magazine, Dr. Oz and News NY 1. Dr. Mitchell also hosts the podcast The Smartest Doctor in the Room – a combination of a lively, personal and in-depth interview with top healthcare specialists.
★ CONNECT WITH DR. MITCHELL ★