My Aching Back – How to Prevent and Treat Back Aches
CONNECT WITH US:
How to Prevent & Treat Back Pain
Back pain is among patients’ most frequent complaints to their doctors. In fact, nearly 65 million Americans report a recent episode of back pain. And about 8% of all adults experience persistent or chronic back pain. And experts estimate that up to 80% of the population will experience back pain at some time in their lives.
Dr. Mitchell speaks with Dr. Stuart McGill, an internationally recognized expert on lower back pain on the best way to be properly evaluated for back pain, holistic ways to get rid of back pain, and why surgery should be the last option.
Where can you get the best medical advice anywhere anytime? I hope on this podcast. Today’s topic is back pain. Just saying those two words make me cringe at times. I can say statistics like one in every four, adults have experienced back pain, but truth be told when you’re the person that has that awful back pain. It’s you, you don’t care about any statistics.
My Personal Battle with Back Pain
I had my own personal battle with back pain. I was a healthy high school and college tennis player who never had any aches or pains could play for hours tennis. And then I got to medical school was where I experienced my first episodes of back pains. And I attributed it to sitting for hours in a classroom. I would be in the classroom from 8:00 in the morning, till five at night, and then more hours sitting on my butt studying to learn anatomy, physiology, all that fun stuff. But the episodes were short-lived, and I usually got better within a couple of days with just some rest and ice and movement.
Then a few years later in medical residency, I was up all night, caring for patients and, and bending over a lot, doing IVs and procedures like lumbar punctures. And again, my back pain came back and this time with a vengeance, it would last for weeks at a time. And that would use all sorts of treatment ice, I went to physical therapy and I was constantly walking around with my lumbar cushion whenever I was sitting in a car or I went to a restaurant. So I can say one thing that looking back that my back pain was actually a blessing in disguise. And you may ask why? Well, it actually was one of the things that pushed me in the direction of holistic medicine. I initially saw an orthopedist for my back pain who put me in a brace and I quickly knew that wasn’t an answer.
I ended up seeking help from physical therapists who were excellent and actually eventually met an osteopath who definitely changed my life with the way he manipulated my back. And he taught me various kinds of exercises that seem to help me a lot. A lot of times too, unfortunately, I was always my worst enemy. I would do certain exercises or seated in a magazine. And before I knew it, the next few days I could barely move.
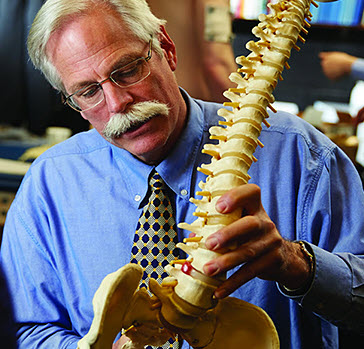
Dr. Stuart McGill, Back Pain Specialist
My guest today. Dr. Stuart McGill is an internationally recognized lower back specialist. He’s a professor emeritus of spine mechanics at the University of Waterloo in Canada. He has researched his entire career, the causes of back pain, and he has worked in treated thousands of patients in his clinic using his exercises. He is the author of several terrific books, which I have, and I’ve read very re-read many times the Back Mechanic, which is one I actually recently read.
I really liked a lot his book, Lower Back Disorders. And I liked for athletes, his Ultimate Back Fitness and Performance. These are all terrific books that show you hopefully under the proper guidance, how to carefully strengthen your back. And although he’s not a medical doctor, I think that’s why so many of his grateful patients are glad that they avoided having to have surgery. He also is now the chief scientific officer at BackFitPro, a company that makes I believe educational and practical products for back pain sufferers. So it’s my pleasure to welcome Dr. Stuart McGill to the podcast.
 Dr. Stuart McGill
Dr. Stuart McGill
Oh, good afternoon, Dean. Thanks for having me.
Who to See for Back Pain?
Dr. Dean Mitchell
My pleasure. Okay. We’re going to get right into it. And probably one of the first, most important questions that any person with back pain has is, who do I go to for my back pain? In the United States, we have lots of healthcare providers that are treating back pain with varying success. We have orthopedists, we have physiatrists or rehab medicine. Of course, we have chiropractors who are doing adjustments, physical therapists. There are osteopaths and acupuncturists. So Dr. McGill I have to ask you. If a friend of yours was across the border in Michigan and called you up and said, “Dr. McGill, I’ve been having back pain for a few months.” Now, who would you recommend I go see first to get an evaluation?
Dr. Stuart McGill
Well, I will create just a little bit of background before I give you the specific answer. And that is Dean, as you know, there’s no such thing as non-specific back pain. That’s like, if you asked me that question, “Oh, I’ve got head pain. Who would you suggest?” Well, we would need a very thorough assessment to understand the mechanism of why you have head pain. We would sub-categorize your head pain and then find you the most appropriate expertise. So I’m going to answer back pain and exactly the same way. But here is the issue. No single profession that I’m aware of. And I’ve worked with them all is trained to do a thorough assessment of back pain.
You have to sub-categorize that person down now to perform a thorough assessment, a very thorough understanding of biomechanics anatomy, neurology, movement, psychology. You have to really know how to probe that pain.
And then the first order of business is to stop the cause. So if you go to your family doc, and you get a pain med, right, you never saw a back pain expert who measured the cause and then intervened at that level. If you go to a surgeon, you are speaking to someone who uses a knife that will hopefully cut out the source of the pain. And I can go through the full litany that way. So, unfortunately, we’ve had to train our own clinicians. We call master clinicians in the McGill method who take several years actually to go through the various schooling and different.
Dr. Dean Mitchell
What is their background? Are they different backgrounds?
We have MDs, chiropractors, physical therapists. We even have a strength and conditioning coach who has met the level of the master clinician. He can read an MRI and I’m sorry to say this, but more effectively than most radiologists, because all of us see the patient first we know and we’ve measured their symptoms. So then when we look at the EMR, we’re calibrated because the picture, the MRI shows the full history of that person’s life. All of the old scars plus the new fresh wounds that are causing pain. And you cannot interpret an MRI until you have the perspective of knowing what that person’s mechanism is. So do you see?
Dr. Dean Mitchell
Yeah, this is a great point. You know what I loved about what you write about your books, Back Mechanic, especially too then, which unfortunately doesn’t happen a lot in the United States because they have so many assistants of assistance taking history and doing this till the doctor strides in, like you said, you watch how the patient enters the room. You watch the patient, how they get up and out of a chair. In the United States, don’t doctors get reimbursed for watching you get up and out of a chair. But you mentioned your books, you learn so much along with a good history of where the problem is emanating possibly from; is that correct? Am I saying that right?
How Dr. McGill Approaches Back Pain
Dr. Stuart McGill
I think so. But there’s a genesis to that. When I started the back pain clinic at the university, I had free rein to start from ground zero. And I thought, how am I going to set up an assessment that is all based on the outcome. We are to be measured on our outcome, not on how many dollars we generate or on how much time we spend, or how many patients we see a day. We will be measured solely on outcome, which is really what the outcome. I mean, nothing else really matters.
I started out setting aside two hours to see a back pain patient. And my medical colleagues said, “Are you nuts? No one spends two hours.” And I said, “how can you not spend two hours? Because it takes me two hours to perform a thorough assessment.” It starts out listening to the story of the person. What are all the impediments that have stopped them from getting addressed and cured by the dozen other clinicians that they’ve seen? And then we perform provocative testing. We create the pain, knowing the specific activities, motions, postures, and loads that create the pain. Then the next order of business is a little bit of a coaching session, which is a little bit of an experiment in progress. If you slouch in a chair and that causes your back pain, but you look up and that causes your right toe to go on fire, that’s a very primary indicator of a near Allender hook on the nerve roots, serving that toe.
Dr. Dean Mitchell
Right? You keep on doing, you don’t realize like all of us, you end up doing the same motions, whether you realize it unconsciously or consciously and in breaking bad habits is difficult.
Dr. Stuart McGill
Right? So anyway, to get down to really answer your question, there isn’t a profession that knows how to thoroughly assess the back. All the way through.

Most people, well, the athletes who come the amateur athletes, they’ll say, “Oh, well I want a personal best. I want to be able to dead lift 200 kilos or something.” And I said, “Really, you do.” I said, “You are history. You’ve got three grown children. Now you’re going to be a grandfather soon is your goal really to be the best rocking grandfather when you’re 65?” Because if that’s your goal going for the next personal best has just decreased your ability of being that rocking grandfather.
So let’s be clear now on what your goals are. So we have a very precise target, and then we are going to choose precise tools, matched to your very precise mechanisms to build the foundation and then progress it to get you there.
Now some physicians and hospitals will say, “Well, we can’t afford to practice like you.” And my answer to that is you cannot not afford to practice because you bill for your time when people fly in from around the world here to get three hours. And for the first time they leave with a very solid direction on what to do 15 minutes. Doesn’t do it.
Best Advice for Getting Diagnosed
Dr. Dean Mitchell
Yeah. It’s interesting. So I’m not sure how it really works in Canada, but it would make so much sense for insurance companies, which control obviously a lot of the access to healthcare in the United States that somebody with back pain seeing you versus going for the MRI or these other testings, seeing three different specialists that financially it would be better for the insurance company. And obviously for the patient to go to somebody like yourself, who’s doing that very extensive evaluation and setting up a program. So, again, the whole issue about it’s not cost-effective. I agree with you. I think it’s cost-ineffective, to having people shifting around. I mean, you should see so many patients who go to… They start having back pain or involved with pain management, which I really don’t like, they’re just getting shot up with, injections and things like that, but I want to get back to one thing though, again.
I know this might be a little hard to pin you down, but if a patient goes to see a provider, but can you remember, they’re going to choose somebody, whether it’s a chiropractor, osteopath, somebody who they associate with treating back pain, do you feel that there are a few things that really should not be overlooked in the physical diagnosis?
Like you see the patient bend forward, checking their spinal curvature, having them do… I mean, can I remember my orthopedic my brief orthopedic training in medical school, like we are crossing the legs over checking for a herniation. Is there anything that you would say to a patient again, just in some simple advice? Again, if somebody just walks in, “Oh, here’s your back pain” and they just look at it and they press a couple of disks. That’s the full extent of the value of the physical exam. Obviously, that doesn’t sound too adequate.
Dr. Stuart McGill

That was the rationale. And in chapter six are nine tests that a person can coach themselves through. And then based on the results of those nine tests, they will know what to do and what not to do for the first time to wind down their pain. So that was why that book was written because they will not get the most simple of what I would consider an assessment to show them what to do and not to do. So you go and see a surgeon and they say, go do yoga, swim or something generic like this. And there’s the yoga may help them. There might be two or three yoga exercises that may help them. And then three that will hurt them. So it doesn’t make sense.
How to Protect Your Back Especially When You Sit All Day
Dr. Dean Mitchell
No, I think the book is great. It’s interesting. You say it was difficult to write. And so it’s funny, in some sense, I would say almost been easy to write only because you were essentially doing this with your patients. It’s like myself when I sometimes, I’m used to speaking to doctors or giving lectures, but I’ve found that over the years when I’ve written a book and written articles, the gear to the laypeople, I just pictured myself that they’re in my exam room and I’m talking to them as if they were just there one-on-one. And that to me helps me write.
All right, let’s move on to something else I want to get to. Because again, I also want to hopefully give listeners some specifics that will be helpful to them. So ergonomics today, so much of our day is sitting in front of a computer, especially on Zoom meetings. I’m doing that now with patients. My patients are doing it for their work or people who like to surf the internet for hours. I want to ask you how we can best protect our backs. And I know you make some points in the book about this. So let’s start with sitting in a chair. Are there certain chairs that really are better than others? I know for myself, there are certain ones that, especially when I was having back pain, there were ones that were much more comfortable than others.
I like the point. I’ll just bring out what you make is that it’s not always so much the position you’re sitting with. It’s moving around. Do you know what I mean? Because you could be sitting in the best posture, but if you’re sitting that way for hours, you’re going to develop problems. So I was wondering if you could give us some pointers on, again, people who are really desk drowned more than before what they should be looking for. Or who they should work with to make sure that again, what they’re doing by sitting not exacerbating or creating back pain.
Dr. Stuart McGill
Well, there are several things to unpack here to get to an answer that will help people. And the first is, I’ve already mentioned, there’s no such thing as non-specific back pain, we need to do the assessment. So we know if sitting and what type of sitting is causing their problems. The second foundational principle is biology does not give you free lunch. It does not give you the infinite capacity to load. Load is magnitude. Load is the frequency of application. Load is duration, which is sitting.
A generic answer to that one is, you cannot sit all day and expect to have a healthy back. But there’re nuances to this.
There are some people, it’s so unfair, they’re just out of shape or condition, couch potatoes, and sitting doesn’t bother them.
And then there’s the poor fella whose conscious of their health, they’re desk-bound for 10 hours a day. And then they go and train hard in the gym.
It’s 17 chapters in the book, but let me give you some examples because you asked here. So let me dispel some myths.
It’s interesting how many people come here and I’ll listen to their story and I’m doing pattern recognition and they’ll say, “Oh, I have tight hamstrings with my back pain and I keep stretching my hamstrings and I sleep in a recliner chair. I watched the TV in this beautiful, comfortable recliner chair.” And I say, that’s why your sciatic nerve is so sensitized.
Get off the recliner. The recliner flexes the hips and extends the knee. You just put a stretch tension on a sciatic nerve, get rid of the recliner.
Get more upright with lumbar support because usually, the upstream source of the sciatic tension will be discogenic. It’s usually a disc bulge or something pathologic with the disc. So there’s one start, stay off the floppy couches. They might be comfortable to you, but they are not de-stressing the spine to allow it to become pain-free.
Dr. Dean Mitchell
Let me ask you to talk about what’s happened now again with ergonomics. I’m sure you’ve heard it or seen it. People now have standing desks. I mean, some people, I don’t know how they do it. They do it on a treadmill. They’re doing their work typing away at a computer, walking on a treadmill. I mean, crazy stuff. That to me doesn’t seem to be very sensible. Like I think people are going to get injured, but what do you think about it, I think it was called Varidesk here in the United States. They have a desk like where, if you’ve been sitting for a while, it has a spring and it elevates so you can actually stand while you’re doing stuff. What are your thoughts about that?
Dr. Stuart McGill
It may be fabulous for a certain type of person. So once again, if we take the typical disc bulge with an open Fischer, that is one where the disc bulge shrinks and grows based on posture, another model.
So here, I’m going to show you if you sit for a long period of time as an open Fisher, so you see the nice juicy.
And now I’m going to squeeze the spine and bend forward and it can sit in. Do you see the little red lamination in the collagen and at the end of my finger Squeeze and flex forward and do you see it open up? And the bulge coming out, trapping the nerve. Now, you stand up in the variable height desk. And now when I squeeze the spine because the spine is not flat when you reflex the hydraulic effort was posterior on the juicy nucleus. Now the whole disc flattens, but notice nothing comes out. So if they have a posterior, the lamination, which most radiologists just call a disc tear, which is just totally inadequate for the detail required, will help the patient then standing up or better yet laying on the tummy will vacuum in that disk bulge, if it’s a very specific type of open Fisher. The bigger, the rounder, the spine, the diameter, the faster it will resorb in the smaller slender spine. That takes more time.
Just watch me get out of a seat here. So now I’ve got my knees together. If I get out of the seat, I’ve got no chance to use proper mechanics. And it might be when I do a hip scour exam, I’ve got lots of room when my knees are spread apart but when my knees are together, I get an impingement. If I sit with my knees apart and get my feet underneath me, my hips can now move. I can de-stress my spine and stand up with zero pain.
Micro-Movements and Back Pain
Dr. Dean Mitchell
Let’s move on to something else too. And again, I apologize if I’m trying to pin you down on certain things. I respect what you’re trying to say. And at the same time, I found, reading your books, little hints that I thought helped me a lot, and the next thing I want to move into, and then this is really important, is stretching. We frequently see professional athletes doing lots of stretching right before the game starts. The weekend warriors, like myself, try to put a little stretching in. We’re not always so great about it. One of the things I learned from your books, which to me was very important. Like I mentioned again, in the intro of the podcast when I was having back pain in residency, it was pretty bad then.
I would get up before work started. And, obviously, from sleeping all night, I was very stiff and it seemed like the pain was at its worst early in the morning. I remember going to see a physical therapist and they would say do stretches. And so I try 15 minutes before I was going to work doing some stresses and I’m like, this doesn’t feel good. And, I remember then reading in your books later on saying that the disc fluid is at its driest early in the morning and that you really better off.
Dr. Stuart McGill
No, It’s the opposite. You’ve given me so much to riff on there.
I’m doing pattern recognition as you’re speaking. So when you tell me, you wake up in the morning and that is the peak of your back pain. I’m going to look at your bed. So you may be laying in a bed that’s too soft, allowing the spine to deviate into your pain. I’ll just give you another sub-category of pain. There is L3, L4, L5. That’s a normal disc and that’s a normal disc. This has lost stiffness and turgor because of the disc injury observed in a twist. Do you see how the majority of the motion is now occurring at the joint that’s lost controlling stiffness. Those are called micro-movements.
So if you lay in bed and the spine deviates with a soft mattress, now you’ve created micro-movements right at that level and the symptoms will show us what level the micro-movement is occurring. Forget about stretching, forget about everything else until you can deal with the primary cause, which was a sleeping posture. But then I know patients come in here and say, my physical therapist, told me when I get out of bed in the morning to lay and pull my knees to my chest.
Here’s what happens. That fires a stretch reflex, which will give an analgesic perception for 15 or 20 minutes to the patient. So they perceive that they’ve done something good. What they didn’t realize was the collagen of their disks is an adaptable fabric. If you keep stretching it, it will become more mobile. I hope you enjoy your pain because you needed the opposite. You needed the collagen to the ground substance between the collagen fibers to stiffen up, stop moving it, stop the stretching, and slowly the pain will wind down, but you won’t stretch that pain away.
Secondly, if it’s a sensitized nerve, you will not stretch the pain away. Now, think of all of the people who come in and they say, Oh, with my back pain, I’ve got tight hamstrings. I stretch my hamstrings all the time. And I say, tell me, how long have you been stretching your hamstrings? Oh, I’ve been doing it for months. I said, and how well does that work for you? Stop stretching your hamstrings. So there would be an argument for that particular subcategory. Stop stretching.
Now let me play the other side of the coin. We’ve measured in certain types of back pain categories, neurogenic facilitation considers having a sore knee. You will limp. That’s what your brain does as facilitation. Your brain causes body parts to limp in your back if you have hip pain and back pain. Those who have this sequelae, shall we say, they may have what we call gluteal amnesia. The brain preferentially decides let’s not activate your gluteals and we’ll get the hamstrings to extend your hip. And that will cause over time, extra stress on the hip and the spine. That is an inhibition of a muscle.
Now here’s the opposite. The brain, if you sit too much and cause discomfort from sitting, generally not in everybody, but the assessment will show, they get neurogenic facilitation, the opposite. The psoas muscle, which crosses the hip in the front, the person gets out of the chair and it’s hard for them to stand up because of the stress. I said, don’t stretch your hamstrings. Now I’m going to say stretch your psoas. So we would take a lunge position. If I can move back far enough here, we’d take a lunge position. I can even palpate the psoas tendon. There, it’s soft. I’ve done a lunge. I’m stretching my hip flexes, but there’s no load on the psoas tendon until I put my hand right up overhead and lean away and drop my shoulder. Now I just felt psoas tendon become tight. So even the stretching technique matters in terms of addressing the real cause. So there is facilitation and inhibition why you might want to stretch and why you must not. It all depends on the assessment.
Dr. Dean Mitchell
Do you have a strong feeling about people waiting till once you’ve been up and moved around and maybe taking a hot shower and you’re looser?
Dr. Stuart McGill
Yeah, because you’re taller when you wake up in the morning than when you went to bed at night, the reason is the discs are hydrophilic. They suck up fluid throughout the night. Throughout the day, hydrostatic pressures from gravity and muscle usage, squeeze fluids out. So if you’re typical, I would measure you would be about two centimeters or almost an inch for you Americans, two centimeters taller when you first get out of bed in the morning. Then when we stress the spine, the discs are like little water balloons. The stress is much higher in them. So when you squeeze them, you’re much more likely to an end plate fracture in the middle of the endplate and not on the edge. That’s a more light, end-of-the-day kind of injury. But some people get up in the morning and they’re just so full of fluid.
Why You Shouldn’t Lay Around with Back Pain & Benefits of Yoga
Did you know that astronauts, for example, when they go into space because gravity is not squeezing fluid out of their spine, so they grow a couple of inches? They get puffy face syndrome as the lymphatics milk fluids back upward without the gravity, which is now absent. Their eyes are pressurized. There’re all sorts of medical complications, they’re on spine pain the whole time. So here now is a person, who we did another experiment, where we put people to bed for eight hours and we measured the hydrostatic stress inside their disks. And then after eight hours, they got up and then other groups we let stay in bed for 36 hours. They’re spines were under so much stress. They were screaming. So, the old days of telling people the rest in bed, I hope you enjoy your pain.
Dr. Dean Mitchell
Because of the old recommendations, especially from physicians, I wouldn’t say it anymore, but in the old days they would say, lay in bed, stay in bed for a couple of days, ice and take some pain meds and you’ll be fine. That was the… I don’t know about Canada, but in the US you know, maybe 15, 20 years ago, that was the standard of care. Let me ask you too about I’ll call them stretches. Some people might call them yoga movements that you recommend in your book, and I’ve used them I think they’re good. The cat-camel pose, where you make the back concave, and convex. Also, something called Cobra, which I think a lot of people are familiar with now. It’s sort of a little bit of a hyperextension. It’s almost like a little bit of a pushup.
And one of the things that somebody shows me, I don’t know, I used to always like it because I really felt that it stretched on my back I think the yoga name is called the plow. Where you bring your legs over your head, and George Sheehan, who was a doctor who led The Running Movement in the United States, like 25 years ago, he used to have what he called his Magic Six. They were a couple of these exercises that he swore helped him avoid injury for the most part in running marathons, he was a big marathon runner. So what about a couple of those stretches overall. Beneficial? You mentioned them in your book. Are they dangerous for anybody? Are they overall safe for people
Dr. Stuart McGill

But my colleague, a fellow named Bernie Clark wrote a book called Your Spine, Your Yoga. And he coaches the person through an assessment of their anatomy and their pain triggers, and there’s a course by Yoga International, where both he and I have collaborated on it for yoga practitioners.
So they know their pain triggers, and they know what yoga exercises are guaranteed to trigger pain and ones will provide.
Dr. Dean Mitchell
That’s very interesting because I know a lot of people that swear by yoga, but I know yoga instructors who some of them have had debilitating back pain. So it’s interesting that you say that because people always thought of yoga as the cure-all for back pain.
Dr. Stuart McGill
Now, having said that, I suggest you go to your hip surgeon, colleagues. There are a few in New York and say what are the demographics of the people in your waiting room? And they will tell you if they’ve studied them, they will be women in their fifties, who’ve practiced yoga for 20 or 30 years now requiring a hip replacement. Is it the fault of yoga? No, it’s partly the fault of the Americanization of yoga that turned it into this game of how far can you stretch.
Versus the original Indian origins which were all about transcending the mind.
Dr. Dean Mitchell
Yeah, I want to bring up something too. And this might be very basic to you, but it was something that I learned over time because I ended up doing over the years, I’ve done some yoga, so it was really interesting when earlier when I had back pain, you see a physical therapist, they would teach you stretches. But the one thing I felt that the physical therapists didn’t do, which yoga did, was teaching you to breathe into a stretch. I don’t know again how you feel about this, but I’ve always found it’s almost like you’re more in tune with your body versus just pushing through something. When you have to breathe into a stretch. I don’t know. I feel like you feel it more, you know what your limitations are. Any thoughts on that?
The St. Louis Cardinals and Predicting Back Injuries
Dr. Stuart McGill
Now you’re getting into the very mindful part of yoga, which we cannot deny.
However, again, some yoga practitioners take this way too far and they start teaching yogic breathing to athletes.
Wait a second. You will be crushed under the basket in the MBA. If you are doing yogic breathing, instead, you must stiffen your core, box out your opponent, and they are waiting for the second for you to do a yogic breath, relax your core, and then they nail you. You are out of position. It is martial arts under there. So again, there’s very little transference from yogic breathing to the field of play. But now I’ve got another surprise for you. We measured the St. Louis Cardinals. They won a little thing called the world series
This little team called the Cardinals, won the world series. Well, the year they won the world series, plus the year before we measured every single player. And this was through my colleagues at the Central Institute for Human Performance in St. Louis. They measured a full fitness profile, strengths, endurance, range of motion, and movement ability. And then for the next two years, we tracked to see which player… By the way, the pitchers were out. And we had the three teams. So we had The Big Show, the Cardinals, and the three AAA teams or whatever they call them. We had 96 players, I believe. And then we saw who got back injury over the next two years, plus any other type of non-traumatic musculoskeletal injury.
Do you know that we were able to predict, I think we had four or five back injuries. I can’t remember. We predicted by doing data mining. Looking at the scores and putting it into an algorithm to see if certain fitness variables and movement profiles conspired together to allow, and I use that word allow, that person to sustain a back injury. And do you know, we were able to predict the four or five with a hundred percent accuracy who had a back injury and even more spectacular we will able to predict with the same algorithm, the 92, who never did get a back injury.
Now, what were the variables? The first variable was hip mobility and how well they were able to move their hips with proximal stiffness and control in their core. So if I want to push and I move my spine, that’s an injury marker. But if I lock my core and give a very athletic push that uses the spine, as it’s meant to be, to give it full sporting potential.
But the other variable was breathing mechanics in a quiet state. So do you see how I have to play both sides of this because it’s very situational dependent.
So that’s why here, I got to bring in the precision and I know you have to teach this to the masses. So you need consumer ability. And that was the struggle in the book.
When is it Appropriate for Spine Surgery
Dr. Dean Mitchell
All right, we’re winding down here, but there’s two last topics I do want to get to. And again, we’ll see if I can pin you down on something. And I think hopefully the answer would be never but, when is it appropriate to have spine surgery? I’m just asking when you’ve seen cases where you say, “Look, I can’t help this person unless they get an operation.”
Again, I’m not a big fan of spinal surgery, most people seem to do very poorly after it. And Tiger Woods unfortunately seems to be one of those cases. Again, I don’t know all the details there, but again, when would you think someone would maybe need spinal surgery?
Dr. Stuart McGill

However, considering surgery is a risk and we want to maximize the reward and minimize the risk ratio, I go through rules. First of all, you have to peg down the surgeon. Can you prove that the thing you’re going to cut out will remove my pain? And if they are doing exploratory surgery, I’d run the other way. If they’re going to work on more than one level, your chance for success of cutting out your pain drops dramatically.
We give plans. You may have been told that … you’ve tried physio, osteopathy, chiropractic, et cetera, and because you failed all of those, the last thing for you is surgery. What a terrible route to surgery.
Dr. Dean Mitchell
And wait, I’m sorry to interrupt you again. It just was the way I used the word surgery, too. And also, I hate to throw in there, is the pain management people. They’re busy implanting these devices in people, and I consider that a surgery when they start putting those stimulators in, that’s a surgical or whatever you want to call it, procedure. Right?
And I’ve rarely seen successes with that. Honestly, with my patients that have gone through that route.
Dr. Stuart McGill
Well, everyone I see is a failure. I’m never the first person they’ve seen. And I’m usually the last straw. But I will say this, we perform virtual surgery. And it’s a program. We precisely define what their pain triggers are, we stop the cause and then I touch them, like I’m knighting them with a sword and I’m saying, “There is your virtual surgery.” Certainly works on many people, because for the first time it’s forced rest. Now, I’ve just heard this woman, she’s a stay-at-home mom, she says, “Every day I have to go to the gym and ride the elliptical trainer for 40 minutes, otherwise, I’ll murder my husband.”
“It’s the way I relieve stress.” And I’ll say, “And that’s why you never get better. You’re an exercise addict. And every day you pick the scab on your back. Go have your surgery.” And it may work because for the first time it’s forced rest.
Now I’m going to perform virtual surgery. There’s your surgery. Now start acting like you’re post-surgical.
You’re going to rest. And I’m going to build a program with short interval walks, we’ll get the various tissues that ought to be moving flossing and moving. We’re going to build some core stability. We’re going to build some strategic mobility in the distal parts of your body. And we’re going to do it in a progression to build you all back up again, just like good rehab should do. Now, this will knock your socks off. We follow up with every patient I’ve ever seen in the entire history of the university. I know exactly our outcome score.
If you have been told that you’ve tried everything and surgery is your last resort. When we do virtual surgery in the way I’ve just described, we have 95% of those people who avoid surgery and in the two-year follow-up are glad that they made that decision.
Well here’s another part in that chapter on Should You Be Considering Spine Surgery. Ask the surgeon what the cause of your pain is. And if they say, “We don’t know what causes back pain,” run the other way.
Learn more about Dr. Stuart McGill on his website backfitpro.com
About the Author – Dr. Dean Mitchell, M.D.
Dr. Dean Mitchell M.D. is a Board-Certified and Immunologist based out of NYC. He graduated from the Sackler School of Medicine and completed training at the Robert Cooke Allergy Institute in New York City. He is also a Professor of Clinical Immunology at Touro College of Osteopathic Medicine, a fellow of the American Academy of Allergy, Asthma and Immunology, and the author of Allergy and Asthma Solution: The Ultimate Program for Reversing Your Symptoms One Drop at a Time. Dr. Dean Mitchell, M.D. has also been featured in The New York Times, The Huffington Post, Fitness Magazine, Dr. Oz and News NY 1. Dr. Mitchell also hosts the podcast The Smartest Doctor in the Room – a combination of a lively, personal, and in-depth interview with top healthcare specialists.
REFERENCES
Rubin Dl. Epidemiology and Risk Factors for Spine Pain. Neurol Clin. 2007; May;25(2):353-71.
Hoy D, March L, Brooks P, et al The global burden of low back pain: estimates from the Global Burden of Disease 2010 study Annals of the Rheumatic Diseases Published Online First: 24 March 2014. doi: 10.1136/annrheumdis-2013-204428
★ CONNECT WITH DR. MITCHELL ★



