Children and Allergies – Everything You Need to Know

Table of Contents
What are Allergies? How Do Allergies Happen?
Are Allergies More Prevalent Today in Children?
How to Know if Your Child Has Allergies
What are the Most Common Allergies in Children?
How to Help Your Child with Allergies
Does Sublingual Allergy Immunotherapy / Allergy Drops Work?
Final Thoughts on Children’s Allergies
What does Johnson’s baby shampoo and Dr. Mitchell’s allergy drop treatment have in common? No more tears!

Most parents have seen the commercial for Johnson’s baby shampoo – the one that prides itself on not causing their children to scream and go into tears as the shampoo inevitably gets into their eyes. Unfortunately, not enough parents are familiar with allergy treatment options for their children that don’t result in tears.
Across the nation, the number of infants, children, and adolescents with allergies continues to rise. In fact, up to 40% of children suffer from allergic rhinitis. And children whose parents have allergies have an increased risk. Allergies make kids miserable with all the nasal congestion, sneezing, and itchy, watery eyes. Parents will do anything to help their children get relief.
This ultimate guide to children’s allergies walks through everything from what allergies are to the most common types of allergies in children to the best ways to treat your child’s allergies.
What are Allergies? How Do Allergies Happen?
Allergies are problems of the immune system. An allergic reaction happens when your body’s immune system overreacts to a benign substance such as tree pollen or pet dander. In other words, your body responds by going into attack mode against an agent that it erroneously perceives as threatening. Normally, the human body defends itself against harmful substances but occasionally it violently attacks mild things like dust, pollen or mold.
When the body sounds the alarm, the immune system goes into self-protection mode – launching a vigorous and violent counterattack against potentially harmful intruders, such as pollen, grains, mold spores, dust mites, animal dander, foods or certain drugs. That overreaction takes its toll on the body and can be likened to getting out the heavy artillery when you’re battling a common housefly.
The single most important fact when learning about allergies is something that Dr. Vincent Beltrani of Columbia University impressed upon me when I was beginning my training to become an allergist – “You’re never allergic to something the first time you get exposed to it.”
What Causes Allergic Reactions?
Over time, and by repeated exposure, the body’s immune system can become “sensitized” so that the body will no longer tolerate a certain agent, even though it was fine when it was exposed to that agent before. The allergen, let’s say a specific food like peanuts or shrimp, is introduced to the body’s immune system which now sees the food as a harmful invader and reacts. The reaction comes out of nowhere, and, as surprising and strange as it seems, people do become allergic to precisely those foods that they regularly consume.
Allergic reactions can affect the eyes, nose, throat, lungs, skin and gastrointestinal tract. Further exposure to that allergen will trigger this allergic response again. Some allergies are seasonal and can only happen at certain times of the year, such as when pollen counts are high, whereas others can happen anytime someone comes in contact with the allergen.
What Causes Allergies in Children?
Below are the six main types of allergy triggers.
- OUTDOOR ALLERGIES
- tree or plant pollen
- insect bites or stings
- INDOOR ALLERGIES
- dust mites
- pet or animal hair/dander
- cockroaches
- INDOOR / OUTDOOR ALLERGIES
- mold
- IRRITANTS
- cigarette smoke
- perfume
- car exhaust
- FOOD ALLERGIES
- any food can trigger an allergic response but the most common allergy-inducing foods include milk, wheat, eggs, soy, fish, and nuts
- MEDICATIONS AND CHEMICALS
Are Allergies More Prevalent Today in Children?
My patients frequently ask me, “are allergies, in general, becoming more common?” The answer is indeed they are. How much have allergies and asthma grown? Figures from the World Allergy Organization reveal the global prevalence of asthma has increased by an astounding 50 percent every decade for the past 40 years. According to the Asthma and Allergy Foundation of America, more than 50 million Americans have experienced various types of allergies each year and allergies are the sixth leading cause of chronic illness in the U.S.
When it comes to kids, allergic conditions are the most common health issues affecting children in the U.S and about 5.9 million or 8% of children have food allergies. And children with food allergies are two to four times more likely to have asthma or another allergic disease.
How to Know if Your Child Has Allergies
Some allergies are easy to identify by the pattern of symptoms that follow exposure to a specific substance while other allergies are subtler and may masquerade as other conditions. The type and severity of allergy symptoms vary from allergy to allergy and person to person. Allergies may present as itchy eyes or as life-threatening anaphylaxis.
Common Signs and Symptoms
The most common symptoms of an allergic reaction include:
- sneezing
- itchy nose and/or throat
- stuffy nose
- itchy, watery eyes
- coughing
- wheezing or trouble breathing
- throat tightness
- vomiting
- itchy rash, hives or itchy welts (atopic dermatitis or eczema)
asthma symptoms such as shortness of breath, coughing, wheezing - red, itchy, dry skin
- upset stomach
- a drop in blood pressure, causing lightheadedness or loss of consciousness
- severe, life-threatening allergic reaction (anaphylaxis) – this can cause trouble breathing, vomiting, diarrhea, low blood pressure, fainting, or death
The Allergic March
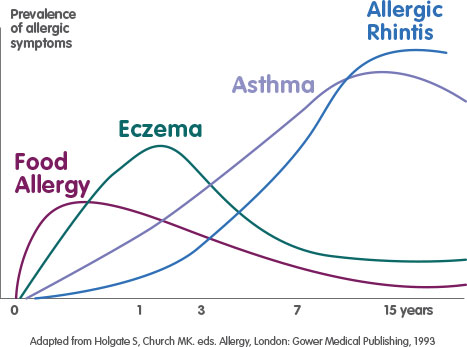
We know that children who are genetically predisposed to develop allergic diseases will generally develop symptoms and signs of disease in a predictable sequence throughout childhood. This staged and expected trajectory has been called the allergic march. The Allergic March describes how young infants and children that present with allergic signs and symptoms: rashes such as eczema, chronic nasal congestion, and runny noses plus possible food allergies can develop later on in life chronic respiratory diseases, such as asthma or chronic sinusitis.
At intervals, an allergic child will first develop eczema in infancy presenting as an itchy, red rash. These infants and young children (under 3 years old) may also develop gastrointestinal symptoms like colic, diarrhea, and abdominal pain or suffer from chronic ear infections. As the allergic child matures, the skin and gastrointestinal symptoms may subside and give way to respiratory symptoms with the development of nasal congestion and asthma. Later on, as we grow toward and through adulthood, allergies cease to follow a straight line, and as a result, they are not always easy to spot. This makes it difficult for us to know that we are allergic, even if the symptoms are in plain view.
Allergy Testing
Going to the allergist for testing today is completely different than experience than it was even just a few years ago. Once upon a time, a patient, even kids, had to endure so many skin pricks to determine their sensitivities that many began to feel like human pincushions. No more. Great advancements have been made that make my job a lot easier and my patients experience less anxiety and discomfort.
Many people fear the allergist, much like the dentist, because they believe they will experience unpleasantness and even pain. But finding out what your child is allergic to is easy and painless.
One of the most advanced tools we have for properly diagnosing an allergy is very low tech: conversation. The allergic evaluation begins with a careful history performed by an allergist to find out the specifics about your child’s symptoms to determine the likely cause. Many of the questions pertain to your current symptoms but there are also questions that seem unrelated but are equally important. A good allergist is adept at playing Sherlock Holmes and the clue that often solves the case may appear in an unexpected place.
Next, is a physical examination in order to narrow down “the suspects.” Following the examination is a simple blood analysis to determine the specific allergy antibodies. It really is that easy. In the past we required skin tests as well, hence all that prodding and poking with scratches. But today’s sophisticated blood analysis allows for precise diagnosis with only one blood draw.
The blood test tells us several important facts.
- It tells the pediatric allergist generally how allergic a patient can be – called total IgE
- The test indicates the likelihood that the patient will develop or has already developed allergic antibodies to environmental substances (pollen, mold, dust) and foods
Is the Blood Test As Accurate As of the Skin Tests? What Are the Benefits of the Blood Test?
All of the recent research indicates both types of testing are highly accurate – close to 90%. Since the two are equally reliable and accurate, I favor the blood test because it has two advantages – safety and standardization. Since you are not introducing the allergic substance into the body, there is no risk of an allergic reaction caused by the test. Also, the blood test is standardized (meaning the lab uses controls to make sure the test is accurate). Skin testing can vary depending on the device used and the practitioner performing and interpreting the test. Additionally, the blood test is not affected by medications like antihistamines.
How Specific Can the Allergy Tests Get?
The testing can differentiate if your child is allergic to cats versus dogs – or if you are allergic to fuzzy hamsters or not-so-cuddly mice. It can even tell you if your child is allergic to horses. Quick summary – the allergy tests can get extremely specific when it comes to pinpointing an allergy.
Where Can Your Child Get Tested?
Today, you can get tested right in your doctor’s office. Pediatricians, primary care physicians, and internists can order these allergy tests. It’s extremely important to diagnose children at a young age. Intervention and proper treatment can affect how allergies develop later in life and, in many cases, can greatly increase the likelihood of effective symptom management, or cause the allergies to subside completely.
What are the Most Common Allergies in Children?
There are a lot of things that could cause an allergic reaction in your child. The most common allergies in kids include:
- Food allergies
- milk
- eggs
- soy
- wheat
- tree nuts
- peanuts
- fish and shellfish
- Seasonal allergies or “hay fever” or seasonal allergic rhinitis
- mold or mildew
- tree, grass and weed pollens
- Dust
- Pet Dander
- Chemical fumes, aerosols, fresh paint, perfume, scented products
- Cockroach droppings
- Tobacco, wood smoke
Food Allergies in Children
With a food allergy, the body reacts as though that particular food product is harmful causing the immune system to create antibodies to fight the food allergen. People often confuse food allergies with food intolerance because they have similar symptoms. The symptoms of food intolerance include burping, indigestion, gas, loose stools, headaches, nervousness or a feeling of being “flushed” but food intolerance doesn’t involve the immune system, can happen because the body can’t digest a substance such as lactose and can be unpleasant but is rarely dangerous.
It’s important to recognize what a food allergy reaction is because it’s not always obvious. Reactions caused by allergies to food run the gamut from rashes to diarrhea to death. The most common food allergies in children involve reactions to milk, eggs, soy products, peanuts, wheat, tree nuts, and fish.
Food allergy reactions can affect any of these four areas of the body:
- skin: itchy red bumps (hives); eczema; redness and swelling of the face or extremities; itching and swelling of the lips, tongue, or mouth (skin reactions are the most common type of reaction)
- gastrointestinal tract: belly pain, nausea, vomiting, or diarrhea
- respiratory system: runny or stuffy nose, sneezing, coughing, wheezing, shortness of breath
- cardiovascular system: lightheadedness or fainting
Food allergy is on the rise. Today 1 in 13 children have a food allergy– and 40% are found to have a severe reaction to the food. Peanut allergy is notorious for causing severe food allergy reactions. Today 1 in 70 children are allergic to peanuts- back in 1997 1 in 250 children had a peanut allergy. The good news is that testing is getting better and safer.
Prevent Peanut Food Allergy in Your Family

The biggest news in the field of Allergy the past few years is the finding that giving peanuts to your infant who you are worried about may develop a peanut allergy is the right thing to do! This contrarian advice actually has some powerful research behind it. The LEAP study, done in multiple medical centers showed that infants at risk for peanut allergy(who don’t have it already) that are given peanut paste at 4 to 6 months of age are 10X less likely to develop a peanut allergy than the infants that are put on avoidance of peanuts.
This fascinating medical mystery points to how important an infant’s immune system can be trained to avoid peanut allergy- and possibly any food allergy. We have to thank Israeli mothers for this medical breakthrough. They were feeding their infants Bamba (a sesame and peanut paste) as soon as they went to solid foods; the researchers were fascinated why Israeli infants and children had much lower rates of peanut allergy than relatives in New York or London. Doctors need to remember: mothers do know best!
New Food Allergy Tests
When I have a concern that a child has a peanut allergy I order the UKnowPeanut test (PIRL labs); this test can quite accurately detect if a child is at risk for a severe allergic reaction to peanut. These tests are more specific than a skin test- and safer because the child gets no exposure to the actual peanut, it’s all through the blood. I’ve also been fortunate to advise parents who were concerned their child might have a peanut allergy that in fact, they were not allergic to peanut from the test. I can also order other food allergy tests in the blood or do skin tests if I think it is necessary.
At Mitchell Medical Group, I have been using with my patients the latest food allergy blood test to diagnose a severe food allergy. The older skin tests are still commonly used by many allergists, but in truth, the newer allergy blood tests called Component testing or for peanut allergies, UKnowPeanut test (PIRL labs) can indicate if someone is allergic to a dangerous protein in the food. With peanuts, these proteins are called Ara h1, 2 and 3. For milk, it is casein and for eggs ovamucoid. There are many foods that can be tested this way and just need a specialist to properly interpret. It’s also a great test to help know if you have just a mild allergy to a food, that is not dangerous.
How to Help Your Child with Allergies
Treatment will depend on your child’s symptoms, age, and general health. It will also depend on how severe the condition is. Conventional treatments, while useful in the short term, and in particular contexts, are meant for occasional usage and are simply not the best long-term solution.
To understand the inherent limitations of traditional allergy treatments, we must distinguish between battling the symptoms of allergy, which some of these medications can do in the short term, and overcoming allergy for life, which none of these medications can promise. A review of the traditional therapies including their individual strengths and shortcomings is essential to arriving at an understanding of the breakthrough in allergy that will relegate all of these to a secondary tier.
Traditional Allergy Treatments
The 3 most popular and traditional ways to treat allergies are avoidance, allergy immunotherapy, and medicine such as antihistamines.
AVOIDANCE
Medications are typically our best line of defense in treating allergies, but the real goal is not to stifle the symptoms but rather to find the underlying cause of the allergy and then remove it so it is no longer a constant source of exposure. That means that once the important detective work is completed and you’ve discovered the source of the allergy, wherever and whenever possible, the next step is to rid your environment of this offending allergen.
Avoidance means staying away from something that gives you an allergic reaction. The allergen(s) your child is allergic to will dictate the type of avoidance that is necessary. For example, if your child is allergic to milk then they will need to avoid all food products containing milk. Below are some common ways to avoid particular allergens:
- During high pollen count or windy days, stay indoors
- Control dust in the home, particularly in your child’s bedroom
- Use air conditioning instead of opening the windows
- In damp areas of the home add a dehumidifier (but remember to clean it often)
- If your child plays outside on high pollen count days, have them take a bath or shower, wash his/her hair and change clothes soon after they come indoors
- Plan vacations in areas where pollen is not as common such as near the ocean
ANTIHISTAMINES / MEDICATIONS
For decades antihistamines have been the first line of treatment for all types of allergic reactions. It’s automatic. If you have an allergy, take Benadryl. Benadryl is a well-stocked staple of every pharmacy, and you’ll find it in almost every person’s medicine cabinet at home – and most certainly in the households of anyone with a history of allergy.
This type of medication is extremely effective at controlling mild, acute allergic reactions such as spontaneous hivelike rash, a sneezing fit, or an itch in your throat. It is safe and effective and indispensable in a pinch but it’s only a “quick fix.” Its duration is limited to a few hours, and it only reverses the allergic reaction at a superficial level, which means it can’t really resolve the problem, but it generally does hold it at bay for short periods of time.
In an attempt to improve upon these classic antihistamines, the drug companies produced what is called the first-generation antihistamines – Seldane, Hismanal (both no longer on the market) and Claritin became top-selling medications. These drugs had the advantage of being longer-acting antihistamines. The problem with all antihistamines is that people develop tolerance to them which means if the medication is needed for weeks or months at a time the body builds up resistance to the medication and it stops providing the same level of relief as it afforded initially.
Managing Allergies at School and on Holidays
At the end of summer, I get lots of calls from parents who have children with allergies who are in school that need their allergy prescriptions filled for the school nurse. The main prescriptions are for the EpiPen, which is the injectable adrenaline used for severe allergic reactions to foods or insect stings. The other prescriptions are for asthma inhalers, in case a child experiences an acute asthma attack. This is routine for my office – but it should be anything but routine for parents whose child needs to have these medications available and be used in case of an allergic or asthmatic emergency.
The Business Section of The New York Times ran a lead article in 2012 entitled: “Tiny Lifesaver for a Growing Worry.” The article focused on how many states (not New York) had passed a law that an EpiPen can be used in a school without a prescription by a school nurse to treat a child in danger of anaphylaxis (the most severe form of allergy). The article showed a picture of how EpiPens would be mounted in the nurse’s office just like a defibrillator unit (to reverse cardiac arrest) to call attention to the use of this life-saving medication. This medical issue unfortunately only got national attention when a year ago, Amarrria Johnson, who had a known peanut allergy was given a peanut by another child and went into respiratory arrest due to the allergic reaction. The nurse did not have a documented prescription to give epinephrine and it was not given in time to prevent America’s death. Law-makers and Health officials using common sense are now putting laws into place to allow a qualified health professional to administer the EpiPen, regardless if a prescription is in place. This is important because a child may develop a severe allergic reaction for the first time in their elementary school years and they may not have had the need for a prescription. A study in Massachusetts found that 25% of children that received epinephrine never knew they had an allergy.
So, once again, if your child has a food allergy please make sure the school has an updated prescription to use epinephrine from your doctor, and the same goes for asthma medications. We also recommend making sure your child has an EpiPen available and ready to go. You can invest in a case like the Veta Smart Case & App for your EpiPen Auto-Injector to monitor the temperature and expiration of the epi-pen but also immediately alert parents when their child has used the EpiPen.
Managing Allergies on Halloween
In our NYC Allergy practice, I see a lot of kids with food allergies, but I have not found a case where a child couldn’t participate in this fun Halloween event if some reasonable ground rules are set before the fun of collecting candy begins.
The key ground-rule for Halloween is that while all candy can be collected:
- No candy is eaten until the child comes home
- Parents must carefully go through the Halloween candy and make sure they don’t contain any nuts
- If the candy is home-made or there is no visible label, then the candy goes into the garbage – no arguments there
- If your child is very young — go with them so they are not tempted to “cheat”
Set firm ground rules for collecting the candy. If a family is throwing a Halloween party and they know that some of the children may have food allergies to nuts, a great place to order nut-free candies and desserts is from Divvies, who specialize in nut-free, great-tasting treats. I personally met the owner, Laurie, and her son, who were on The Martha Stewart Show last spring when I appeared and their nut-free candies and desserts are an excellent option.
Allergy Immunotherapy – The Allergy Solution
Band-Aids versus the Solution
The difference between traditional allergy treatment and allergy immunotherapy is not merely semantic and it will change the lives of those with allergies. Traditional allergy treatments can go only so far in helping allergy sufferers because at best they are able to offer only transitory relief from the symptoms of allergy. Now we have the tools to not only quiet the symptoms but also to reverse the underlying condition.
How Allergy Immunotherapy Works
The mechanism behind allergy immunotherapy is simple and elegant. The treatment is analogous with lifting weights. We all know that working out is good for us but the only way to get stronger is to lift more weight. The more often we do so, the stronger we become and the more efficiently our bodies operate.
Similarly, in allergy immunotherapy, a person’s immune system builds up protective blocking antibodies when the patient receives gradual, stronger doses. The stimulation in the immune system creates a shift in the immune balance to block allergy symptoms instead of developing such symptoms.
The concept of allergy immunotherapy is that the immune system can be taught not to overreact. With immunotherapy you start with the tiniest doses and expose the patient to the very allergen he/she is allergic to, and then very gradually build-up to the higher and higher doses until the patient’s body builds a tolerance to the allergen. By building a tolerance to the allergen, the immune system is learning to tolerate and to stop overreacting to what should be a harmless substance. The beauty of this treatment is that it truly is a natural treatment – you are receiving a substance that you are allergic to and allowing your immune system to solve the problem.
Allergy Shots / Injections
Allergy shots or injections are the most common form of allergy immunotherapy. Allergy shots were the most effective form of treatment we originally had because they addressed the allergic response itself, not just the symptoms.
Although allergy injections are for the most part extremely safe, the process quickly delivers the allergen into the bloodstream which can trigger a potential allergic reaction and carries the risk of a severe or anaphylactic response. An anaphylactic response or systemic reaction as allergists call it to allergy shots happen when the body is overactivated by an injection of allergy vaccine and the body releases massive amounts of histamine. These reactions can be severe and even fatal.
Sublingual Allergy Immunotherapy – the Alternative to Painful Injections
Making allergy immunotherapy into an orally administered treatment makes more sense because of the safety factor. The sublingual route takes advantage of direct absorption (but in a slower fashion than an injection) into the venous bloodstream through the mucosa (tissue) under the tongue. The medicine, or in this case allergen, is absorbed without being destroyed by the enzymes in the stomach.
The beauty of allergy drops versus injections is that you are getting small, safe doses daily, but at the same time, your body is getting a quantity of medication that is one hundred times higher which leads to immune protection.
The cornerstone of this treatment is that patients receive increasingly higher concentrated dilutions so that they can build a protective lasting immunity. The real advantage is that this treatment is custom-tailored to each patient and can be done at home. With allergy injections, the compliance is around 30-40% due to the need to come into the allergists’ office each week for shots. Allergy drops work so well because patients use them regularly and have a 90% compliance rate.
Sublingual Allergy Immunotherapy Protocol – How Soon Will My Child Feel Better?
The protocol for sublingual allergy immunotherapy or allergy drops is very simple. Once your child has been tested to determine which substances they are allergic to then the allergist makes a specific allergy vaccine to allow the body’s immune system to develop protection to the allergen and make a vaccine that is tailored to your child’s specific allergies. It is not a one-size fit all approach.
Allergy drops are safe for young children and they can take the drops daily at home with only a few in-office appointments needed per year. During the first year of treatment, your child should feel noticeably better. But, by the second year, your child should not only feel even better but allergic parameters will also show that your child is indeed better by a medical definition.
After three years, patients on allergy drops immunotherapy have received the maximum benefits and further drops are typically not necessary. In other words, the current thinking is that you need to continue treatment until your child has received the maximum protection level.
Does Sublingual Allergy Immunotherapy / Allergy Drops Work?
The principle behind why the sublingual allergy drops treatment works is exactly the same as with the more traditional injection therapy, but instead of being administered through shots, the sublingual treatment is given through oral drops placed under the tongue.
Recent Studies
The studies keep pouring in: at the American College of Allergy, Asthma and Immunology meeting in Phoenix, researchers presented data showing that sublingual allergy tablets to grass pollen were safe and effective in children. This was the first study done in North America. Prior studies were done in England and Europe. The exciting part is that the therapy appears to work within 16 weeks and gave significant protection against grass pollen allergy compared to placebo (water tablet). It is also easy for kids to use.
I’ve been using the sublingual method to treat my patients for the past decade and have seen the dramatic improvement in children and adults. Dr. Blaiss, a former president of the Allergy society, mentioned that the great thing about this therapy is that it changes the immune system to protect against the allergen, unlike drugs which can only try and mask symptoms. I wrote in my book, Dr. Dean Mitchell’s Allergy and Asthma Solution: The Ultimate Program for Reversing Your Symptoms One Drop at a Time, that this unique therapy which has been around for over twenty years in Europe can change the lives of millions of allergy and asthma sufferers.
Journal of Allergy, Asthma, and Immunology Study
One more important recent study: in the “The Journal of Allergy, Asthma and Immunology” in November 2015, a team of top Italian allergy researchers showed that if patients continued their allergy drops for the proper maintenance period of 3 years, they kept their protection for over 8 years and beyond. This again goes to prove that immunotherapy is an immune changing treatment that can give long-lasting protection. The most striking other fact is that patients receiving the drops developed no new allergies during the therapy, whereas the control group (just meds, no drops) had a 24% increase in developing new allergies.
Patient Story
I had in my office a wonderful, beautiful 7-year-old girl with brown, curly hair. Her smile could light up a room, but when her mom told me that she was getting allergy shots from another allergist in town her face became sad and tears started to roll down her eyes. She wanted to get better from her allergies, but getting weekly shots was just as miserable.
I was able to bring a smile to this young girl’s face when I told her that I don’t use shots to treat allergies; instead, we make up allergy drops that you place under the tongue to desensitize to different allergens. This young girl was highly allergic to dogs and desperately wanted to have a dog of her own.
Allergy Drops: A no-brainer
It’s really a no-brainer anymore: for environmental allergens (cats and dogs, tree and grass pollens, dust mites and molds) allergy drops are the way to go. I just can’t wait until the food allergy studies that are currently underway come out. Allergists and their food-allergic patients so desperately need a safe treatment option.
When to See a Pediatric Allergist?
If your child’s symptoms are not alleviated with over-the-counter medications like Benadryl or other allergy medications, it is time to see a pediatric allergist. A pediatric allergist can take a simple blood test and medical history to determine if your child is suffering from allergies and pinpoint the exact allergens that are causing allergic reactions. While many people choose to use over-the-counter medication to help their kids’ fight allergies we believe that finding the underlying cause of the allergy and treating the cause is the best approach.
What to Expect at Your Appointment
Here’s what you can expect at your first appointment with a pediatric allergist.
- Allergy test (some allergists still use a skin test to identify allergies. I recommend finding an allergist who utilizes a blood test instead)
- Conversation including the careful medical history of your child
- Physical examination
In my opinion, one of the most advanced tools used to properly diagnose allergies is extremely low-tech – conversation. Make sure you choose an allergist who will spend enough time with you and your child to get a thorough medical history and any other pertinent information to diagnosing their allergy.
Why find an allergist who uses a blood test to detect allergies over a skin test:
- Safety. There is no risk of an allergic reaction because this test doesn’t introduce the allergic substance into the body.
- Standardization. Blood tests are standardized which means the lab uses control to make sure the test is accurate. Skin testing can vary by device and practitioner interpreting the test.
- Medication doesn’t affect the blood test but medications like antihistamines do impact the skin test results if not stopped at least 48 hours prior to the test.
Final Thoughts on Children’s Allergies
Allergies don’t have to make your child and you miserable. Just like Johnson’s tear-free baby shampoo, there are is a great pain-free and tear-free allergy solution available for kids – allergy drops!
My book, Dr. Dean Mitchell’s Allergy and Asthma Solution: The Ultimate Program for Reversing Your Symptoms One Drop at a Time, published over a decade ago gives in-depth research as to how safe, convenient and effective allergy drops are for environmental allergens. It’s a home-based program that is easy to do – and no more tears. The drops actually a slightly sweet taste and easy to administer.
I can’t figure out why every pediatrician is not telling their patient’s parents that this is the best way to not only reverse allergies but to prevent future allergies.
The sublingual allergy drops work to stop allergies to pets (dogs, cats-even horses), to pollen, mold and dust mites. These are the common allergens that cause allergic rhinitis, allergic conjunctivitis, and allergic asthma.
The latest breakthrough is that these allergy drops can now be used to treat dangerous food allergies to peanuts, tree nuts, milk, egg, soy, and shellfish.
About the Author – Dr. Dean Mitchell, M.D.
Dr. Dean Mitchell, M.D. is a Board Certified Allergist and Immunologist based out of NYC. He graduated from the Sackler School of Medicine and completed training at the Robert Cooke Allergy Institute in New York City. He is also a Clinical Assistant Professor at Touro College of Osteopathic Medicine, a fellow of the American Academy of Allergy, Asthma, and Immunology, and the author of Dr. Dean Mitchell’s Allergy and Asthma Solution: The Ultimate Program for Reversing Your Symptoms One Drop at a Time. Dr. Dean Mitchell, M.D. has also been featured in The New York Times, The Huffington Post, Fitness Magazine, Dr. Oz and News NY 1. Dr. Mitchell also hosts the podcast The Smartest Doctor in the Room – a combination of a lively, personal and in-depth interview with top healthcare specialists.
This site contains affiliate links to products. We may receive a commission for purchases made through these links.
References
Dr. Dean Mitchell’s Allergy and Asthma Solution, Dean Mitchell MD. Marlowe and Company, 2006. Dr. Dean Mitchell’s Allergy and Asthma Solution: The Ultimate Program for Reversing Your Symptoms One Drop at a Time
Allergy Relief for Your Child, U.S. Food & Drug Administration. https://www.fda.gov/consumers/consumer-updates/allergy-relief-your-child
Allergies in Children, Cedars-Sinai Medical Center. https://www.cedars-sinai.org/health-library/diseases-and-conditions—pediatrics/a/allergies-in-children.html
All About Allergies, reviewed by Jordan C. Smallwood, MD. KidsHealth from Nemours. https://kidshealth.org/en/parents/allergy.html
Why So Many Allergies – Now?, Gwen Smith in Food Allergy. Allergic Living, November 20, 2010. https://www.allergicliving.com/2010/11/20/allergies-why-so-many-now/
Allergy Facts and Figures. Asthma and Allergy Foundation of America. https://www.aafa.org/allergy-facts/
CDC.gov. (2018). FastStats. [online] Available at https://www.cdc.gov/nchs/fastats/allergies.htm
Allergic March photo courtesy of https://www.startwell.nestle.com.my/ms/nankidr-optipror-ha#



